The University of San Francisco
USF Scholarship: a digital repository @ Gleeson Library | Geschke
Center
Doctoral Dissertations Theses, Dissertations, Capstones and Projects
Spring 5-1-2024
THE ASSOCIATION BETWEEN UNCERTAINTY, REPRODUCTIVE DISTRESS, AND AVOIDANCE IN ASSIGNED FEMALE AT BIRTH ADOLESCENT AND YOUNG ADULT (AYA-F) CANCER SURVIVORS
Devon Ann Pons
University of San Francisco, [email protected]
Follow this and additional works at: https://repository.usfca.edu/diss
Part of the Health Psychology Commons
Recommended Citation
Pons, Devon Ann, “THE ASSOCIATION BETWEEN UNCERTAINTY, REPRODUCTIVE DISTRESS, AND AVOIDANCE IN ASSIGNED FEMALE AT BIRTH ADOLESCENT AND YOUNG ADULT (AYA-F) CANCER SURVIVORS” (2024). Doctoral Dissertations. 628. https://repository.usfca.edu/diss/628
This Dissertation is brought to you for free and open access by the Theses, Dissertations, Capstones and Projects
at USF Scholarship: a digital repository @ Gleeson Library | Geschke Center. It has been accepted for inclusion in
Doctoral Dissertations by an authorized administrator of USF Scholarship: a digital repository @ Gleeson Library |
Geschke Center. For more information, please contact [email protected].
THE ASSOCIATION BETWEEN UNCERTAINTY, REPRODUCTIVE DISTRESS, AND AVOIDANCE IN ASSIGNED FEMALE AT BIRTH ADOLESCENT AND YOUNG ADULT (AYA-F) CANCER SURVIVORS
A Clinical Dissertation Presented to
The University of San Francisco
School of Nursing and Health Professions
Department of Health Professions
Clinical Psychology PsyD Program
In Partial Fulfillment of the Requirements for the Degree
Doctor of Psychology
by
Devon A. Pons, MS, CCLS
July 2022
TABLE OF CONTENTS
Chapter
I. ABSTRACT
II.INTRODUCTION AND CRITICAL LITERATURE REVIEW
Statement of the Problem
Critical Literature Review
AYA Survivorship
Uncertainty
Oncofertility and Reproductive Distress
Avoidance 19
Purpose and Rationale of the Study
Research Questions and Conceptual Hypotheses
Clinical and Theoretical Relevance
Definition of Terms
III. METHODS
Research Design
Participants
Procedures
Description of Measures
Data Analysis
IV. RESULTS
Descriptive Statistics
Bivariate Analysis
Main Analysis
Exploratory Analysis
V. DISCUSSION AND CONCLUSIONS
Implications
Limitations
Suggestions for Future Research
Conclusion
VI. REFERENCES
VII.TABLES AND FIGURES
Table 1:Frequencies of Demographic Characteristics
Table 2:Frequencies of Medical Characteristics
Table 3:Descriptive Statistics and Correlationsof Variables of Interest
Table 4:Frequencies of Responses to Avoidance Items
Figure 1:Path Model without Control Variables ShowingStandardized Effects
Figure 2:Path Model with Control Variables ShowingStandardized Effects
Figure 3:Path Model without Control Variables Showing Standardized Effects
Figure 4:Path Model with Control Variables ShowingStandardized Effects
VII. APPENDICES
Appendix A:Socio-demographic Information
Appendix B:Medical History
Appendix C:Reproductive History
Appendix D:Reproductive Concerns After Cancer Scale(RCACS)
Appendix E:Impact of Events Scale – Revised (IES-R)
Appendix F:Decisional Self-Efficacy Scale (DSE)
Appendix G:Uncertainty Response Scale (URS)
DEDICATION AND ACKNOWLEDGEMENTS
I would like to thank my committee for all of the time and support put into guiding me along this dissertation journey. In particular, I would like to thank Dr. Catherine Benedict who graciously shared her data and infinite knowledge base with me regarding the world of AYA survivorship.
Most importantly, I send my deepest gratitude and love to my family near, far, and in the classroom. Your presence, cheerleading, and support has been everything this socially driven extrovert needed to buckle down in solitude to complete this feat.
It’s us (three) now.
AYA-F UNCERTAINTY, REPRODUCTIVE DISTRESS, AND AVOIDANCE
Chapter I
ABSTRACT
Family building and fertility is a complex component of survivorship for assigned female at birth Adolescent and Young Adult’s (AYA-F’s), often accompanied by a mix of cognitive uncertainty, emotional uncertainty, reproductive distress and avoidance. Whenever these psychological components present in survivorship for AYA-F’s they can impact coping, identity development, and individualized care plans throughout survivorship. This novel examination of data from a cross sectional study shed light on the associations between reproductive distress, uncertainty, and avoidance and how they are experienced differently by various subgroups within the sample.
Results demonstrate that reproductive distress fully mediated the association between emotional uncertainty and avoidance, while no association was demonstrated between cognitive uncertainty either directly or indirectly through reproductive distress. When controlling for age, age at diagnosis, education level, household income, and decisional self-efficacy, the mediation between emotional uncertainty and avoidance through reproductive distress was no longer observed (although emotional uncertainty and reproductive distress were still associated) and no other significant associations were found amongst the main psychological variables of interest. However, there were significant findings between age at diagnosis, household income and self-efficacy with reproductive distress as well as between self-efficacy and avoidance.
These results implicating decisional self-efficacy with avoidance adds to existing literature on avoidant behavior predictors for AYA-F’s specifically. By better understanding these associations, survivorship experiences and individualized fertility related support needs are now better understood and the standard of care for AYA-F’s in survivorship can be better tailored to the nuanced psychosocial needs identified within this study.
AYA-F UNCERTAINTY, REPRODUCTIVE DISTRESS, AND AVOIDANCE
Chapter II
INTRODUCTION AND CRITICAL LITERATURE REVIEW
Statement of the Problem
There are over 370,000 female adolescent and young adult (AYA-F) cancer survivors in the United States, the majority of whom have a high likelihood of becoming long-term survivors (Young et al., 2019). Fertility research has demonstrated that these same survivors have an increased risk of not conceiving within a year of their initial attempt by comparison to the general population (Young et al., 2019), secondary to well-established data demonstrating gonadotoxic cancer treatment effects on reproductive health, ovarian failure, and pregnancy complications (Benedict et al., 2016; Benedict et al., 2020; Logan et al., 2019). Cancer and treatment-related effects on reproductive function depend on a number of factors such as age, diagnosis, and treatment method, which often lead to uncertainty about reproductive health outcomes after treatment is completed.
The practice of fertility preservation prior to treatment has become a widely researched and discussed component of person-centered oncology care for AYA-F’s due to gonadotoxic treatment effects that render survivors at risk for infertility, difficulty conceiving or carrying a pregnancy, or shortened reproductive timeframes (Benedict et al., 2020; Canzona et al., 2021; Innarino & Palmer-Wackerly, 2021; Ussher & Perez, 2019). While a push to have fertility discussions with this vulnerable population prior to treatment has become more standardized, less is known about the support efforts and impact for these same patients after treatment has concluded, when family building becomes more salient (Benedict et al., 2020; Quinn et al., 2016; Shay et al., 2017).
AYA-F UNCERTAINTY, REPRODUCTIVE DISTRESS, AND AVOIDANCE
Additionally, research demonstrates that the low incidence of cancer in AYA’s by comparison to pediatrics and older adults renders the medical care system insufficient in treating the psychosocial nuances for this population (Benedict et al., 2020; Crook et al., 2016; Ford et al., 2013; Halliday & Boughton, 2011; Mertens & Gilleland Marchak, 2015; Shay et al., 2017). In existing survivorship care, AYA’s being treated by an oncologist reported higher unmet fertility related needs by comparison to AYA’s who receive their follow up care from their primary care physician (Shay et al., 2017). In fact, approximately 45.4% of polled AYA’s report unmet needs related to fertility after cancer, including those seen in oncology and primary care settings, which was among the top areas of commonly reported unmet needs (Shay et al., 2017). This research demonstrates that both current generalized and oncology specific survivorship practices are not meeting the psychosocial needs of the majority of AYA-F’s considering family building after treatment.
Simultaneous to these systemically unmet needs, the common coping mechanism of avoidance employed by survivors to help manage emotional uncertainty, cognitive uncertainty, and reproductive distress may also exacerbate their already unmet needs. In choosing to avoid discussions (with providers or others) in an effort to move on from their cancer experience or avoid associated challenges to improve immediate coping, survivors may perpetuate the cycle of not addressing fertility and family building discussions with providers as well. This avoidance may be explained by Hua and Howell (2020) report that, “the cognitive, affective, and behavioral underpinnings of information avoidance point to a broader factor underlying avoidance: a sense that one cannot cope with the cognitive, affective, and behavioral implications of bad news” (p. 2). If a system is not addressing fertility needs and the survivors are avoiding these same discussions in an effort to maximize coping through maintaining hope or avoiding threat, there is
AYA-F UNCERTAINTY, REPRODUCTIVE DISTRESS, AND AVOIDANCE
risk that the already narrowed fertility window for survivors will be further negatively impacted by ongoing avoidance.
Ultimately, research demonstrates that the majority of survivors express the desire to have children of their own (Benedict et al., 2019), and the long-term health impacts around potential risk to fertility has been demonstrated to be one of the most distressing components of survivorship; which can lead to healthcare information avoidance as a means of coping with the related distress and uncertainty (Barton et al., 2013; Benedict et al., 2020). While avoidance is already demonstrated to be impacted by self-efficacy of coping, relational support levels, risk perception, trait anxiety, age, gender, and intersecting social determinants, more research is needed to understand how uncertainty and reproductive distress may impact avoidance as well (Aldaz et al., 2019; Chae, 2016; Hua & Howell, 2020; Jung et al., 2013; Lipsey & Shepherd et al., 2019; McCloud et al., 2013; Orom et al., 2021; Sweeney et al., 2010). To address this gap, this is the first study, to the author’s knowledge, to explore how uncertainty and reproductive distress relate to avoidance of fertility and family-building issues among AYA-F survivors in an effort to empirically inform survivorship support services for AYA-F’s.
Critical Literature Review
AYA Survivorship
In 2020 alone, there were approximately 89,500 new cancer diagnoses in adolescents and young adults (AYA’s) ages 15 to 39 years (American Cancer Society, 2020). The most prevalent type of cancer diagnosed within this AYA range varies depending on age of diagnosis, but most commonly includes blood, thyroid, skin, lymphoma and solid tumor cancers (American Cancer Society, 2020). The specific diagnosis, modality of treatment, and the age at which someone was treated for cancer is closely related to long-term health outcomes (Mertens & Gilleland Marchak,
AYA-F UNCERTAINTY, REPRODUCTIVE DISTRESS, AND AVOIDANCE
2015). Females have a higher incidence of cancer rates than their male counterparts starting from the age of 20 years (American Cancer Society, 2020). While females have slightly lower mortality rates than men, rising overall incidence rates in AYA-F cancer diagnosis are attributed to a plethora of genetic, environmental and dietary factors (American Cancer Society, 2020; Wong et al., 2017). Fortunately, overall mortality rates for AYA’s are decreasing, which consequently increases the number of AYA survivors each year (Logan et al., 2018; Wong et al., 2017). Once AYA’s are diagnosed with cancer, they are considered in survivorship for the duration of their life (National Cancer Institute, 2009).
The mental health experience of AYA-F’s is impacted by many factors and can be challenging to understand as the majority of research either focuses on childhood or adult cancer survivors instead of the unique subset of AYA’s specifically (Mertens & Gilleland Marchak, 2015). Research has demonstrated that in general, female survivors, those from lower SES backgrounds, and those who have a family history of anxiety or depression are considered at risk for increased mental health challenges in survivorship (Benedict et al., 2016; Mertens &
Gilleland Marchak, 2015). Due to developmental considerations that implicate the importance of adolescents and young adults building autonomy and decision-making abilities in the AYA age range, these stunted sequelae of developmental tasks can also lead to challenges with a healthy emotional experience in survivorship (Benedict et al., 2016; Pillet, 2010; Shay et al., 2017). While severe psychopathology has not been linked to survivorship, an impact on quality of life and distress has been demonstrated (Ford et al., 2013).
This unique subset of cancer survivors may experience atypical impacts to their developmental progression given health-related interruptions during their adolescent, emerging, and young adulthood developmental stages. According to Erik Erikson’s psychosocial
AYA-F UNCERTAINTY, REPRODUCTIVE DISTRESS, AND AVOIDANCE
developmental theory, individuals ideally progress through a hierarchy of developmental stages throughout life; where adolescents focus on exploring their autonomy, individual interests, define who they are based on school, work and social accomplishments, and draw comparisons with peers as key components to identity formation while young adults explore intimacy versus isolation (Beyers & Seiffge-Krenke, 2010).
These key developmental milestones may be impacted during an AYA’s cancer treatment when parental figures impede autonomous decision making by driving complex healthcare decision making and through continued management of daily-living tasks for the adolescence in treatment or by inversely forcing AYA-F’s to make complex decisions before they would be expected to based on developmental stage. This interruption in typical autonomy development is significant because it may cause AYA survivors to under-develop the independent medical decision making and investigation skills necessary to broach a plethora of future healthcare related decisions or may force them to face decisions about their future when they may be developmentally unprepared to (Innaro & Palmer-Wackerly, 2021; Sansome-Daly & Wakefield, 2013). Additionally, instead of exploring social, professional, and recreational interests that can impact one’s ego and identity development, a survivor may be solely focused on their cancer experience and treatment which may lead to singular identification as a “survivor,” with subsequent underdevelopment of other parts of their identity. According to Mertens and Gilleland Marchak (2015), “cognitive and physical vulnerabilities related to the cancer experience and any current late effects of treatment may impact adolescent survivors’ ability to face these developmental challenges and increase the risk of developing psychological problems in this period” (p. 88).
AYA-F UNCERTAINTY, REPRODUCTIVE DISTRESS, AND AVOIDANCE
Depending on the level of developmental arrest, AYA’s may have not established the ego and self-reliance necessary to be successful in intimate relationships (Beyers & Seiffge-Krenke, 2010). An example of the interwoven impact of identity on intimacy is illustrated by Logan and colleagues (2018) who argue that impacted body image and lack of normalcy can lead to long term impacted sense of self and romantic isolation related to “feelings of being ‘damaged goods’, inadequate or that their body was ‘disgusting’” (p. 26). Such perceptions of self may easily transpose onto challenges with intimate relationships. Considering the biologically time sensitive nature of family building, many AYA survivors often must face fertility-related medical needs and decisions before they are ready based on their stage of development. At the same time, AYA’s report unmet support and education needs related to possible late-effects, cancer recurrence, fertility impacts, ongoing symptoms, mental health considerations, social and romantic impacts, and employment domains which are all relevant during this developmental stage (Logan et al., 2018; Wong et al., 2017).
AYA’s life experiences and development are unique and need to be treated so. They continue to need individualized treatment that is closely aligned with and sensitive to their specific life stage throughout survivorship, yet their own developmental trajectory may undermine their needs for close follow up care if they lean on avoidance of information to follow normative identity development focus on school, work, peers, and romantic relationships over treatment specific considerations (Ford et al., 2013; Smits-Seemann et al., 2017). Given the demonstrated lasting psychological effects of diagnosis and treatment in AYA’s, individualized care is necessary for the remainder of a survivor’s life (Donovan et al., 2015; Mertens & Gilleland Marchak, 2015). While survivorship services do exist for AYA’s, and the Children’s Oncology Group (COG) outlines standards of follow up care specifically for childhood cancer, survivors’
AYA-F UNCERTAINTY, REPRODUCTIVE DISTRESS, AND AVOIDANCE
survivorship services vary (Mertens & Gilleland Marchak, 2015; Benedict et al., 2020). Pediatric and adult clinics who serve a majority of patients outside of the AYA window may not specifically focus on the age-specific needs of this population including fertility and family building, as well as identity development and intimacy/relationships. Without individualized survivorship services, AYA’s unique needs are left unaddressed and underserved by the existing model of treatment in either pediatric or adult survivorship clinics (Goman et al., 2018; Mertens & Gilleland Marchak, 2015; Shay, 2017). As demonstrated by Ford and colleagues (2013), survivors are unlikely to understand their risk levels of post-treatment effects. These factors all implicate the need for specifically tailored survivorship services for the AYA subgroup of survivors. According to Donovan and colleagues (2015), “among the possible causes to which NCI attributes the lack of improved health outcomes for AYAs are the limited awareness of and thus the limited systemic solutions for the challenges unique to this population” (p. 703). Uncertainty
Uncertainty responses pertaining to illness was a concept studied by Mishel (1990) and defined as the inability to make meaning of illness events and outcomes due to insufficient understanding or information. According to Barbour and colleagues (2012), uncertainty exists when information or situations are ambiguous or when not all information is known. Uncertainty has been identified as a predominant psychosocial experience that can be perceived both positively and negatively for those with a chronic illness (Brashers et al., 2003; Woodgate & Denger, 2002). These assessments of uncertainty result in varying behavioral activation depending on how the uncertainty is appraised (Halliday & Boughton, 2011). Such behavioral responses “represent people’s tendencies to seek or avoid health information given their cognitive and affective evaluations of uncertainty” (Carcioppolo et al., 2016, p. 979). Research
AYA-F UNCERTAINTY, REPRODUCTIVE DISTRESS, AND AVOIDANCE
by Chae (2017) has investigated intolerance of uncertainty (IU) and found that those with high IU are more likely to experience anxiety. Subsequent research has linked anxiety to cancer information overload which was demonstrated to lead to maintenance behaviors to promote ongoing uncertainty as a method of information avoidance (Chat et al., 2016; Chase, 2016).
The two components of cognitive and emotional reactions to uncertainty are imperative to understand when investigating the experience and behavioral responses related to uncertainty. Emotional uncertainty is the experiential emotional or affective reaction to situations that are ambiguous and cognitive uncertainty is focused on the thought responses in anticipation or reaction to an event that elicits uncertainty (Greco & Roger, 2001). Research by Greco and Roger (2001), who developed the Uncertainty Response Scale (URS), indicated that while emotional uncertainty was found to be correlated with experiencing anxiety and sadness, cognitive uncertainty was more likely to result in “tolerance of ambiguity” suggesting that those who experience higher cognitive uncertainty would be more apt to seek information or experience less distress from such scenarios (Greco & Roger, 2001, p. 530). The different experiences of emotional versus cognitive uncertainty and its impact on avoidance is imperative to understand further.
Two theories will be employed to understand uncertainty in the context of health care decision making and behavioral activation: uncertainty management theory and the tripartite model of uncertainty (Barbour et al., 2012; Benedict et al., 2020; Brashers, 2001; Cacioppo et al., 2016; Donovan et al., 2015; Greco & Roger, 2001; Hillen et al., 2017; Miller, 2014; Orom et al., 2021). According to Brashers (2001), Uncertainty Management Theory, uncertainty can be experienced both positively and negatively. When uncertainty is experienced negatively, it can cause distress, worry, and avoidance of potentially important information sources or scenarios
AYA-F UNCERTAINTY, REPRODUCTIVE DISTRESS, AND AVOIDANCE
(Chae et al., 2016; Hillen et al., 2017; Orom et al., 2021). This is of importance because feelings of uncertainty and fear of receiving bad news are demonstrated to be the most prevalent concerns related to medical decision-making (Shay et al., 2018). When uncertainty is appraised positively, continued uncertainty can be a coping tool used to maintain an optimistic outlook given that knowing more information about cancer and its effects can sometimes undermine hope (Barbour et al., 2012; Brashers, 2001; Canzona et al., 2021; Cacioppo et al., 2016).
The tripartite model of uncertainty modeled from Brashers and colleagues’ (2003) framework, indicates AYA’s experience of uncertainty falls within three predominant domains: medical, personal, and social uncertainty (Benedict et al., 2020; Donovan et al., 2015). While most healthcare related experiences of uncertainty can be categorized as medical uncertainty, the cancer experience can cause uncertainty in all three domains of the tripartite model (Benedict et al., 2020; Brashers, 2001; Donovan et al., 2015). Benedict and colleagues (2020) have since updated the original model based on fertility and family building experiences. Using AYA-F’s experience with uncertainty about fertility and family building as an example of how all domains can be impacted, uncertainty could be elicited by not knowing treatment or disease impact on a survivors’ fertility. Personal uncertainty of whether a survivor places importance on having children biologically and the social uncertainty of having to manage family building uncertainty with one’s partner or support system could both also be relevant. This indicates that AYA-F’s who are addressing family building considerations are likely faced with all domains of uncertainty outlined by the tripartite model of uncertainty which comes with added complexity (Benedict et al., 2020).
These various appraisals of both emotional and cognitive uncertainty related to medical impact and decision-making being the dominant stressor has implications for how AYA-F’s
AYA-F UNCERTAINTY, REPRODUCTIVE DISTRESS, AND AVOIDANCE
experience uncertainty related to fertility and family building. Research of the AYA-F survivorship population demonstrates that uncertainty related to fertility and family building reportedly stemmed from insufficient information and a lack of understanding of relevant information from providers (Canzona et al., 2021). Halliday and Boughton (2011) highlight the existing gap in literature and indicate the importance of determining the significance of uncertainty as it relates to distress in order to meet the needs of AYA-F survivors specifically. Given this demonstrated need, this research aims to identify how uncertainty and reproductive distress related to avoidant behaviors related to fertility and family building.
Onco-Fertility and Reproductive Distress
The term “oncofertility” was developed by Dr. Teresa Woodruff of The Oncofertility Consortium of interdisciplinary professionals in 2006 to capture all fertility and family building aspects for cancer survivors (Woodruff et al., 2021). Counseling about disease and treatment impact on fertility and fertility preservation options have become a recommended standard of care, suggested by the American Society for Clinical Oncology and the American Society for Reproductive Medicine (American Cancer Society, 2020; Quinn et al., 2016; Young et al., 2019). AYA-F’s should ideally be presented with the opportunity to freeze their eggs or embryos, undergo ovarian transportation, or to do ovarian tissue cryopreservation for those that have yet to undergo puberty before they start oncology treatment (American Cancer Society, 2020; Woodruff et al., 2021). While these options should be discussed with AYA-F’s upon diagnosis, undergoing such procedures may delay the start of oncology treatment, have significant financial implications, and require additional decision making during an already emotionally heightened time (Benedict et al., 2016; Campbell & Hillemeir, 2021). Research by Logan and colleagues
AYA-F UNCERTAINTY, REPRODUCTIVE DISTRESS, AND AVOIDANCE
(2019) demonstrated that such discussions and support needs persist from diagnosis through survivorship given the reported range of negative emotional experiences brought about by threatened infertility throughout the course of ongoing treatment and survivorship.
A national poll conducted by Shnorhavorian and colleagues (2015) indicated that 50% of AYA-F’s did not discuss preservation with their providers prior to starting treatment and of survivors who did not undergo fertility preservation, 38% of AYA-F did not do so in part due to being unaware of their preservation options, 19% of AYA-F cited financial constraints, 55% reported health related concerns and 33% cited interpersonal concerns. Only 6.8% of studied female AYA-F survivors reported making arrangements for fertility preservation (Shnorhavorian et al., 2015). Research by Ford and colleagues (2013) also indicates that approximately 66% of survivors have some sort of late-effects from treatment, such as early menopause as an example, that may impact fertility. Being young and female also implicates higher levels of unmet fertility information needs, so the AYA-F population is at particular risk of not getting adequate support around their fertility journey (Shay et al., 2017). Despite such complexities, the desire for biological children is not influenced by the cancer experience. As such, many AYA-F survivors continue to want a family due to their lack of understanding of treatment-related infertility risks (Barton et al., 2013; van Dijk et al., 2018).
There is a myriad of ways AYA-F survivors may be impacted by infertility, which is sometimes attributed to the disease itself or due to treatment (e.g., surgery, chemotherapy, radiotherapy, or from bone marrow transplantation) that results in gonadal damage or risks associated with pregnancy (Logan et al., 2019). Given these potential impacts cancer treatment has on reproductive health, AYA-F’s may need to consider alternative family building options including reproductive medicine like invitro-fertilization (IVF) via fresh, frozen, or donated
AYA-F UNCERTAINTY, REPRODUCTIVE DISTRESS, AND AVOIDANCE
gametes or surrogacy, adoption, or fostering (Benedict et al., 2020). These alternative family building methods may be sources of uncertainty and distress as many survivors may not have ever considered nontraditional family building measures, may not have thought through their own personal values and priorities related to these options, or may be unsure of the processes involved (e.g., laws and regulations surrounding surrogacy and adoption) and likelihood of success.
For AYA-F cancer survivors, naturally occuring uncertainty related to fertility and family building is well documented to be compounded by the potential impact cancer treatment may have had on their fertility or ability to safely carry a pregnancy, as well as uncertainty about long-term cancer-related risks such as recurrence or other late effects (Wong et al., 2017). The uncertainty surrounding whether treatment rendered a survivor infertile or not and the implications on family building decisions can result in reproductive distress for individuals within the AYA-F population (Benedict et al., 2016). Reproductive distress is linked to anxiety and concern related to one’s ability to build a family which may ultimately impact quality of life, particularly for those who do not already have children (Ussher & Perez, 2019). Research done by Young and colleagues (2019) indicated that 44% of their AYA-F participants reported moderate to high reproductive distress in survivorship, with those who received pretreatment fertility counseling reporting higher levels of reproductive distress. This research may be interpreted to indicate that current counseling efforts are still not comprehensively addressing the support and psychoeducation needs for AYA-F survivors.
To understand the multifaceted components that can lead to reproductive distress, it is also imperative to identify additional considerations. As pointed out by Benedict and colleagues (2020), there are additional layers of uncertainty such as financial implications when considering
AYA-F UNCERTAINTY, REPRODUCTIVE DISTRESS, AND AVOIDANCE
assisted reproductive methods, surrogacy, or adoption should natural conception be impossible or unlikely. AYA-F’s must also manage the ongoing “concerns about impact of cancer on future health, citing concerns for their future health and the health of possible future children” which remains in question after treatment (Canzona et al., 2021, p. 1386). There is also a demonstrated relational impact that AYA-F’s must manage amongst the other stressors brought on by potential infertility (Hawkey et al., 2021; Innaro & Palmer-Wackerly, 2021; Ussher & Perez, 2019; Young et al., 2019). In addition to the relational component, cancer and treatments can also have an impact on sexual functioning itself which can further compound reproductive distress (Wenzel et al., 2005).
This ongoing reproductive distress throughout survivorship is pertinent to an AYA-F survivor’s wellbeing. If an AYA-F decides to avoid fertility discussions as a means of coping with their reproductive distress, that may lead to “uncertainty and confusion that may contribute to future decisional regret or magnify feelings of loss” (Canzona et al., 2021, p. 1383). While avoidance is a natural response when managing distress and can be effective in the short-term, avoidance in the long-term may present challenges (Aldaz et al., 2019). The chronic nature of reproductive distress and implications on a survivor’s identity further the case for why emotional and education supports should be incorporated into standard survivorship practice (Young et al., 2019).
Reproductive stressors and their impact are chronic, as noted by Canzona and colleagues (2021), who indicate that fertility potential can impact AYA-F’s overall wellbeing. Uncertainty about fertility can be exacerbated by inconsistent support and communication on the topic from medical professionals, leading to unaddressed reproductive distress, which may then lead to avoidant coping (Young et al., 2019). Research indicates that when providers neglect
AYA-F UNCERTAINTY, REPRODUCTIVE DISTRESS, AND AVOIDANCE
conversations about fertility, AYA’s report more uncertainty or the belief that infertility risk may be low (Canzona et al., 2021). This research puts the owness on providers to ensure that proper education and support is delivered in order to minimize misconceptions, reproductive distress, and uncertainty to minimize the likelihood of survivors to avoid these discussions themselves. When these proactive discussions are not initiated by providers, survivors’ uncertainty about fertility tends to magnify barriers to fertility discussion (i.e., embarrassment), which may lead to an increased reliance on avoidance as a coping mechanism (Canzona et al., 2021). Delayed care and education may be biologically too late if avoidance persists past a woman’s fertile window, therefore, proactive support and education practices to minimize reproductive distress and confusion should consistently take place (Benedict et al., 2020). Fortunately, these downfalls in oncofertility care have been recognized and the aforementioned Oncofertility Consortium is currently working to expand access, financial support and insurance coverage, advance research, innovate preservation methods for people across the gender spectrum, and provide specific road maps for providers to minimize reproductive distress for survivors (Woodruff et al., 2021).
Avoidance
Avoidance is a common practice in the face of a distressing event and is often conceptualized as a coping tool, communication method, or behavioral response (Barbour et al., 2012; Orom et al., 2021; Sweeney et al., 2010, Shi 2019). It is defined as “any behavior intended to prevent or delay the acquisition of available but potentially unwanted information” (Sweeny et al., 2010). It can be activated fluidly over time where people employ it at certain points during a distressing event, but not at others (Jung et al., 2013; Sweeny et al., 2010) and can be either a conscious or automatic behavior (Howell et al., 2016). It can also serve as either an adaptive or maladaptive coping mechanism to deal with uncertainty related to potential health risks (Hua &
AYA-F UNCERTAINTY, REPRODUCTIVE DISTRESS, AND AVOIDANCE
Howell, 2020) and can be employed to manage the negative affect elicited by potential health threats (Orom et al., 2021). This can materialize as a defense mechanism that leads to the avoidance of seeking out information or avoiding exposure to potentially threatening information (McQueen et al., 2013; Orom et al., 2021).
Efforts have been made to understand why people engage in avoidance. One explanation is that avoidance is an adaptive behavioral response to uncertainty of one’s personal health status (Barbour et al., 2012; Chae, 2016; Carcioppolo et al., 2016; Hua & Howell, 2020). Within certain limits, avoidance can be beneficial as it maintains a sense of hope and optimism in the face of health risk uncertainty (McCloud et al., 2013). Different from knowledge dismissal, avoidance can be intentionally utilized as a communication tool to express explicit avoidance of information that may not align with one’s values or that may elicit negative emotions (Sweeny et al., 2010). When avoidance persists to a degree where personal decision making regarding one’s overall health or health goals are jeopardized, it may indicate a maladaptive coping tool (Hua & Howell, 2020). Depending on how an individual perceives the risk level related to certain health information, they may either avoid or seek knowing more information dependent in part on their self-efficacy (Aldaz et al., 2019; Orom et al., 2021; Shi, 2019).
Current research is also investigating who is likely to avoid. Chae (2016) deduced that avoidant behavior is especially likely for those survivors with trait anxiety. Such trait features can impact how individuals experience new health related information as demonstrated by Chae (2016), who found that highly anxious individuals were more likely to feel overloaded by cancer information. This led to avoidance of cancer information because of confusion and stress. Additionally, people with lower perceived self-efficacy in their coping abilities were also found
AYA-F UNCERTAINTY, REPRODUCTIVE DISTRESS, AND AVOIDANCE
to avoid more often (Hua & Howell, 2020; Orom et al., 2021). Cultural and demographic factors also play an important role in investigating who is more likely to employ avoidant behavior. For example, research by McCloud and colleagues (2013) demonstrated that young females are a population most likely to avoid in the face of potentially challenging healthcare information. Intersectional social determinants have an impact on these behaviors as it’s been demonstrated that people often mirror familial patterns of information seeking or avoidance (Jung et al., 2013). People may also engage in avoidance to manage impressions of those around them by not learning information that may be deemed as undesirable (Lipsey & Shepherd, 2019).
Considering a survivor’s medical history with the barrage of threatening cancer diagnosis and treatment related information along with research about who is most likely to avoid in the face of challenging healthcare instances, it is reasonable to posit that AYA-F’s are likely to avoid, at some level (McCloud et al., 2013; Orom et al., 2021). Whether they aim to only learn information that aligns with their family building values (Sweeny et al., 2010), to maintain hope around family building (Carcioppolo et al., 2016), avoid fertility discussions to manage interpersonal impressions (Lipsey & Shepherd, 2013), or because they have already experienced cancer information overload (Chae et al., 2016), there are many reasons AYA-F’s may employ avoidance as it relates to fertility and family building information.
Given that AYA-F’s continue to have follow up care requirements in survivorship, such appointments are touchpoints that could serve as support opportunities to address post treatment fertility status and plans. However, despite these useful opportunities, research indicates that adolescents reported an underdeveloped understanding of fertility risk and “described avoiding talking to providers as a method for coping with uncertainty” (Canzona et al., 2021, p. 1390).
AYA-F UNCERTAINTY, REPRODUCTIVE DISTRESS, AND AVOIDANCE
Consequently, as pointed out by Canzona and colleagues (2021), this increased avoidance of fertility related discussion with providers can impact levels of depression, anxiety, and emotional support seeking, as well as increase the risk of experiencing fertility-related problems and being unable to achieve long-term family-building goals.
Purpose and Rationale of the Study
Many first-line cancer treatments are identified as gonadotoxic, which may pose fertility challenges or render a survivor infertile once they beat cancer (Benedict et al., 2016). Due to this potential impact, AYA-F survivors are subject to feelings of uncertainty, which may be experienced positively or negatively, and distress about family building in survivorship, which can be anxiety provoking and lead to avoidance as a coping tool (Halliday & Boughton, 2011). While avoidance as a coping tool is a common way to manage healthcare related distress, it can be problematic for AYA-F’s who seek to have children if it leads to avoiding fertility information, discussions, or considerations long enough to miss their already narrowed window for reproduction or the time sensitive decision making to plan for future family building (Benedict et al., 2020). Therefore, it is important to begin to investigate the psychological experience and behavioral responses of AYA-F’s in order to inform targeted psychosocial intervention development for this population. By better understanding the impact of both emotional and cognitive uncertainty and reproductive distress on avoidance, an interdisciplinary support team would be able to provide nuanced support and education to AYA-F’s before biological abilities further narrow with age and time in survivorship. This research is a novel addition to the limited health research regarding post treatment reproductive distress, experience, and behavioral responses.
Research Questions and Conceptual Hypotheses
AYA-F UNCERTAINTY, REPRODUCTIVE DISTRESS, AND AVOIDANCE
Understanding how reproductive distress, emotional and cognitive uncertainty, and avoidance interact will ideally assist healthcare professionals in offering targeted and effective family building and fertility psychoeducation and support services for AYA-F survivors. To identify any association between these variables and specifics about the sample, quantitative analysis of archival data were conducted. The identified research questions were:
1. To what extent does reproductive distress mediate the relationship between both emotional and cognitive uncertainty and avoidance of fertility and family-building information among AYA-F survivors?
2. How are various features of the sample associated with avoidance? It was hypothesized that reproductive distress would partially mediate the association
between emotional and cognitive uncertainty, and avoidance both in the original path model with the primary psychological variables of interest and after controlling for age, age at diagnosis, education level, household income, and decisional self-efficacy. Specifically, it was hypothesized that AYA-Fs with high reports of emotional uncertainty and high reproductive distress would be likely to also index high on avoidance of health-related information about their fertility for a myriad of underlying reasons. Additionally, it was hypothesized that AYA-F’s with reports of cognitive uncertainty and reproductive distress would also be likely to employ avoidance of health-related information about their fertility. For those who do not endorse reproductive distress, existing uncertainty is still hypothesized to be associated with avoidance behaviors. When considering the potential impact of age, age at the time of diagnosis, household income level, education level, decisional self-efficacy, cancer type, and fertility preservation practices, it was hypothesized that older participants would have decreased avoidance, younger
AYA-F UNCERTAINTY, REPRODUCTIVE DISTRESS, AND AVOIDANCE
participants at time of diagnosis would display higher levels of avoidance, that those with cervical, ovarian, or uterine/endometrial cancer diagnoses would endorse higher levels of avoidance than those with other cancer types, and that those who did not undergo fertility preservation will be more likely to report avoidant tendencies. Those that identified as lower income and education level were hypothesized to have higher levels of avoidance than those who were more established financially and completed more schooling. Finally, those with higher levels of reported decisional self-efficacy were hypothesized to have lower levels of avoidance despite levels of uncertainty or reproductive distress.
Clinical and Theoretical Relevance
The clinical implications of this proposed research informs and advocates for empirically indicated support and education practices in survivorship clinics. An understanding of the experience of uncertainty, reproductive distress and avoidance will offer the opportunity for clinicians to better understand how potential associations impact avoidant behaviors. Additionally, the covariates investigated in this research will offer further nuance in the understanding of a profile of patient who is likely to endorse avoidant behaviors. These associations are essential to understand so that AYA-F’s who may want to build families are adequately supported in preemptively addressing their fertility and family building questions and concerns before it is biologically too late. Guided by professionals, AYA-F’s can be supplied with increased support and information to reduce potential cancer information overload and negative avoidant behaviors in survivorship (Chat et al., 2016). Research on this topic will also inform providers on which patients in particular need to discuss fertility and family building concepts in survivorship to remit maladaptive avoidance, despite the demonstrated discomfort in discussing intimate details such as fertility and sexuality with AYA-F’s (Gorman, et al., 2018).
AYA-F UNCERTAINTY, REPRODUCTIVE DISTRESS, AND AVOIDANCE
This research will ideally minimize some of the unique psychosocial stressors that AYA-F’s face in survivorship.
Theoretically, this work will contribute to the dearth of AYA-F specific literature around the impact of uncertainty and reproductive distress on avoidance. Given the unique identity and developmental considerations for this age range, it is essential to understand the specific experiences and behavioral responses seen in this population to assist in the conceptualization and understating of their unique experiences. This work will also expand existing literature on avoidance as it pertains to reproductive considerations specifically and whether cognitive or emotional uncertainty are specifically related to avoidance in distressing situations related to fertility.
Definition of Terms
● AYA-F: Adolescent and young adult female (AYA-F) cancer survivors are defined by the National Cancer Institute as individuals between the ages of 15-39 years old at the time of their diagnosis (2020). Living with cancer in this particular age group elicits distinct psychosocial experiences, stressors, and support needs (Canzona et al., 2021). To encompass women that are having children later in modern day life, AYA-F in this study refers to individuals between the ages of 15-45 years (Benedict et al., 2019).
● Emotional & Cognitive Uncertainty: Greco and Roger (2003), who created the Uncertainty Response Scale, investigated various types of uncertainty, among those being emotional and cognitive uncertainty. Emotional uncertainty includes measures of emotional responses as a consequence of uncertainty such as anxiousness, fear, happiness, or discomfort (Greco & Roger, 2003). Cognitive responses to uncertainty are related to the appraisals of the uncertain situation which could be perceived as both
AYA-F UNCERTAINTY, REPRODUCTIVE DISTRESS, AND AVOIDANCE
positive and negative (Hillen et al., 2017). Research indicates that emotional uncertainty is more likely to lead to maladaptive coping as it’s related to anxiety and sadness, where cognitive uncertainty correlates with higher levels of tolerance to ambiguity and uncertainty (Greco & Roger, 2001).
● Reproductive Distress: Distress related to fertility levels and family building abilities is referred to as reproductive distress. According to Halliday and Boughton (2011), fertility can be a chronic stressor that leads to elevated uncertainty and increased stress levels. Reproductive distress can also result in decisional regret around not having addressed reproductive preservation options or investigating one’s own reproductive values early in their care (Canzona et al., 2021).
● Avoidance: According to the uncertainty management theory, avoidance is understood as an intentional defensive communication response to uncertainty with the aim of remaining ignorant for the purpose of either increasing or decreasing the experiences related to uncertainty as a coping mechanism (Barbour et al., 2012; Canzona et al., 2021; Chae, 2017; Donovan et al., 2015; Orom et al., 2021).
Chapter III
METHODS
Research Design
This archival data analysis was conducted on data from a mixed methods study by Benedict and colleagues (2020) that investigated AYA-F’s post treatment experiences, unmet needs, self-perception, and decision making related to fertility and family building. A total of 111 AYA-F survivors completed a quantitative survey and a subset of survivors completed in depth interviews. A novel analysis of this cross-sectional archival data examined the mediating effects
AYA-F UNCERTAINTY, REPRODUCTIVE DISTRESS, AND AVOIDANCE
of reproductive distress on the association between uncertainty and avoidance of fertility and family building in AYA-F survivors. The original research and recruitment procedures were approved by the Northwell Health Institutional Review Board.
Participants
The original data were collected via multiple recruitment strategies at multiple medical centers and through social media channels of young adult cancer patient organizations over an 18-month span of time. The eligibility criteria included: (1) female gender; (2) English-speaking; (3) aged 15–45 years old; (4) completed potentially gonadotoxic cancer treatment including systemic chemotherapy, pelvic radiation, or surgery affecting reproductive organs; (5) have not had a child since diagnosis (full-term pregnancy with live birth in patient/survivor or surrogate or adoption); and (6) report either uncertainty or a desire for children in the future. From the 485 female cancer patients between the ages of 15-45 years old identified to meet the eligibility criteria, 258 were screened, and 111 AYA-F’s completed the survey used for this study (Benedict et al., 2019).
Procedures
Eligible AYA-F’s were identified through two hospital based centers and via social media recruitment in alignment with IRB-approved methods given its large reach. Electronic medical records from both Northwell Health Monter Cancer Center and the Cohen Children’s Cancer Center were used to identify participants that met the eligibility criteria. Patients’ providers were contacted to provide approval to reach out to their patients, and then eligible parties were sent a letter and given follow up phone calls to obtain consent and confirm eligibility (Benedict et al., 2019).
AYA-F UNCERTAINTY, REPRODUCTIVE DISTRESS, AND AVOIDANCE
The social media recruitment was done through 1-2 posts on various young adult cancer patient organizations social media pages. The four organizations that allowed a total of six total advertisement and recruitment posts on their Facebook and Instagram accounts were: Stupid Cancer, The Samfund, Allicance for Fertilty Preservatoin, and Lacuna Loft. Interested individuals were directed to input their contact information online and then were sent a letter (via email for this group) followed up with a phone call to obtain consent and confirm eligibility. Email correspondence was also conducted with those that opted into research opportunities from the Susan Love Foundation.
The research team first confirmed eligibility criteria and then obtained consent from all participants. The principal investigator obtained informed assent and parental consent specifically for participants between the age of 15-17 years old. After consent was obtained, participants in the original research study were led to an online survey hosted by Research Electronic Data Capture (REDCap) to fill out a demographic and health history related questionnaire as well as the quantitative survey of measures. If requested, participants were mailed a paper copy of the questionnaire. The same research assistant that conducted the initial recruitment follow up phone calls also tracked participants participation in the REDCap survey and followed up with anyone necessary. All participants in the quantitative portion of the study were compensated with $10.
For any participants that voiced distress related to completing the survey, the principal investigator and Northwell Zucker Hillside counseling services were available for support as needed. Additional reproductive life planning resources were also provided for interested participants.
Description of Measures
AYA-F UNCERTAINTY, REPRODUCTIVE DISTRESS, AND AVOIDANCE
Uncertainty Response Scale (URS) (see Appendix G)
The URS utilized in this study is an adapted 10-question measurement that assesses individuals coping strategies and responses to uncertainty. The original measure has emotional uncertainty (EU), desire for change, and cognitive uncertainty subscales. Only 5 questions from both the cognitive and emotional uncertainty subscales were used in the current study. Responses are on a 4-point Likert scale from “Never” to “Always” with higher raw scores indicating higher levels of uncertainty. The alpha coefficients for each subscale ranged from 0.85-0.90, showing good reliability (Greco & Roger, 2001). Research by Greco & Roger found evidence of concurrent validity in that EU was related to high levels of neuroticism. EU was also related to low self- esteem, emotional rumination, and a lack of detachment from stressful situations. Cognitive uncertainty was correlated with tolerance of ambiguity via planning ahead and information seeking (Greco & Roger, 2001, p. 530).
Reproductive Concerns After Cancer Scale (RCAS) (see Appendix D)
The validated RCACS measure utilized is an 18-item questionnaire about AYA-Fs’ concerns about future fertility and reproductive health in survivorship (Gorman et al., 2019). The six subscales address concerns about fertility potential, partner disclosure, child’s health, personal health, acceptance, and becoming pregnant (Gorman et al., 2014). Responses are on a 5-point Likert scale from “Strongly Disagree” to “Strongly Agree.” It is scored by adding up the raw scores, with higher scores indicating higher levels of reproductive concern. The RCAS has good overall internal consistency (a = .82), along with the six three item subscales (a’s = .78 .88).There is also evidence for convergent and divergent validity using the known-groups approach (Gorman et al., 2019, p. 1545). Composite reliability for each of the six subscales
AYA-F UNCERTAINTY, REPRODUCTIVE DISTRESS, AND AVOIDANCE
ranged from 0.66 to 0.87 with “becoming pregnant” being the lowest and “fertility potential” having the highest reliability (Gorman et al., 2019). Impact of Event Scale – Revised (IES-R) (see Appendix E)
The original IES-R is a 22-question scale that measures various aspects of subjective impact of a distressing event (Weiss, 2007). The adapted IES-R utilized in the original study used 8 questions from the IES-R to specifically assess avoidance, while omitting the intrusion and hypervigilance questions. The participants were instructed to fill out this scale specifically in relation to infertility risk. Responses are on a 5-point Likert scale from “Not at all” to “Extremely.” Although used widely in oncology research, this measure was originally developed to align with post traumatic stress disorder (PTSD) criteria in the DSM-IV and is not used singularly for diagnosis. It can be scored using a raw score or via deducing mean scores for each subscale. While the psychometrics of the IES-R are lacking in available research, research with emergency personnel demonstrated a coefficient alpha from 0.84-0.85 for avoidance specifically, demonstrating high internal consistency (Creamer et al., 2003). The original IES by Horowitz and colleagues (1979) demonstrated a Cronbach alpha of 0.82 for avoidance, a satisfactory test-retest reliability of 0.79 for avoidance, and internal consistency of this subscale with a coefficient of 0.92 (Weiss, 2007).
Control Variables:
Sociodemographic data on participants’ age, race, ethnicity, religion, education, employment status, income, and locality were collected. Medical characteristic data were also gathered on participants’ cancer type, staging, therapies, menstrual information, pregnancy history, and family building intentions. Information was also collected regarding participants’ decisional self-efficacy (DSE scale) around making informed decisions.
AYA-F UNCERTAINTY, REPRODUCTIVE DISTRESS, AND AVOIDANCE
The DSE scale (see Appendix F) derived from Bandura’s concept of self-efficacy, which encompases the “coping capabilities and skills in managing one’s motivation, emotional states, and thought processes” (Bandura, 1994, p.83). The DSE scale is an 11-item instrument that measures one’s confidence in their ability to make informed decisions or collaborate with healthcare professionals in decision making, which impacts the more broad concept of self-efficacy (Bunn & O’Connor, 1996). Responses are on a 5-point Likert scale from “not at all confident” to “very confident,” with higher scores indicating greater self-efficacy in decision making. This scale has been demonstrated to have adequate internal validity as evidenced by the range of reported Chronbach’s alpha (0.78 – 0.92) (O’Connor, 2002; Miano, et al., 2020).
Data Analysis
IBMSPSS 28.0 was used to generate thorough descriptive statistics on the demographic characteristics of the sample, to conduct missing data analyses, and to test for assumptions required for path analyses. Bivariate analyses were then conducted between the continuously scaled variables (i.e., RCACS scores, IES-R avoidance scores, DSE scores, URS cognitive uncertainty scores, URS emotional uncertainty scores, age, and age at diagnosis) and pairwise deletion was utilized to handle any missing data. Simultaneous regressions were conducted to examine the relationships between twelve dichotomous cancer diagnosis types and two outcomes: avoidance and reproductive distress. Independent samples t-tests were conducted to determine if those who underwent fertility preservation had different emotional uncertainty and avoidance scores from those who did not undergo fertility preservation.
Prior to running the path analyses, the data were screened and assumptions were checked. Univariate outliers were identified in SPSS by generating standardized residuals and using the
AYA-F UNCERTAINTY, REPRODUCTIVE DISTRESS, AND AVOIDANCE
cutoff of +/- 3 SD units (Bowen & Guo, 2012; Kline, 2015). Multivariate outliers were identified in SPSS by examining Cook’s distance (cutoff of 1) and Mahalanobis distance and associated p values (cutoff of .001; Bowen & Guo, 2012; Kline, 2015). Acceptable relative scaling was also checked by examining covariances with a cutoff of 10 (Kline, 2015). Each variable was also screened for issues with non-normality by examining skewness and kurtosis before examining the normality of residuals resulting from a linear regression with all of the variables included in the model (Bowen & Guo, 2012). Finally, the data was also screened for issues with homoscedasticity and multicollinearity (Bowen & guo, 2012; Kline, 2016). Because the assumption of multivariate normality appeared to be met, MLE was deemed an appropriate estimation method for path analyses, and nonparametric estimation methods (i.e. Bayesian estimation) were not necessary (Arbuckle, 2021a).
The primary research question examining the mediating effect of reproductive stress on the relationships between independent variables (IVs), emotional uncertainty and cognitive uncertainty, and dependent variable (DV) avoidance, was tested by estimating a path analysis model. A path analysis model is a structural model that is identified using only manifest variables and associated error terms for endogenous variables (Byrne, 2016). In this initial path analysis, all endogenous variables are correlated in the model, and paths were drawn between each independent variable (i.e., emotional uncertainty and cognitive uncertainty), a mediator (i.e., reproductive distress), and a dependent variable (i.e., avoidance; see Figure 1). Correlations were tested via Pearson’s correlation. In order to examine direct and indirect effects, the model was also run with bootstrapping for cases without missing data.
AYA-F UNCERTAINTY, REPRODUCTIVE DISTRESS, AND AVOIDANCE
The second model also incorporated five control variables (i.e., age, age at cancer diagnosis, education, household income, and self-efficacy) by including them as additional endogenous variables with paths drawn to the mediator and the DV (see Figure 2) (Hayes, 2022; Becker et al., 2016; Becker, 2005). Standardized estimates, confidence intervals, and observed significance values were examined and reported for the model. Direct, indirect, and total effects were estimated in order to test the research question using bootstrapping for the cases without missing data. Significant indirect effects between the IVs and the DV were evaluated to indicate the presence of a mediating effect by reproductive distress. Direct effects were also examined and, along with indirect effects, were used to determine whether mediating effects should be considered full- or partial-mediation.
Post hoc analysis was performed to modify each path model to obtain goodness of fit statistics and more parsimonious path models (see Figure 3 & Figure 4). In both models, the non significant path between cognitive uncertainty and avoidance was removed. In the second path model with control variables, all non significant paths from the covariates to either the mediator or outcome were also removed. The comparative fit index (CFI; > .90) and root mean square error of approximation (RMSEA; < .08) goodness-of-fit statistics were used to evaluate model fit and compare models (Byrne, 2016; Perry et al., 2015) after removing the aforementioned non-significant paths from both original path models.
Through exploratory analysis of the data, investigation into the patterns of participant behavior and psychological experiences was conducted to create a preliminary profile of patients who are most likely to endorse avoidance. To identify such patients, the significant psychological
AYA-F UNCERTAINTY, REPRODUCTIVE DISTRESS, AND AVOIDANCE
variables of interest in the main path model (i.e. reproductive distress and emotional uncertainty), the control variables (age, age at diagnosis, education level, household income, and self-efficacy), and additional medical considerations (cancer type and fertility preservation status) were reviewed in relation to avoidance. In depth descriptive statistics were run on the impact of events scale (IES-R) to better understand the nuances of avoidance in this sample (see Table 4). Individual item analysis was also conducted using spearman’s rank correlations test to assess individual questions from the URS, RCACS, and DSE scales in correlation with avoidance.
Chapter IV
RESULTS
Descriptive Statistics
The sample consisted of 111 AYA-F, for whom the demographic characteristics are summarized in Table 1. The average age was 30.98 years (SD = 5.49) at the time of taking the survey, while the average age at diagnosis was 24.04 years (SD = 8.10). The majority of the sample identified their race as White (78.5%), followed by more than one race (7.5%), and then as black (5.6%). Of the entire sample, 18.2% identified as Hispanic/Latinx. A total of 46.8% of the sample had a college degree, followed by 36.0% had a postgraduate degree, and 17.1% had less than a college degree. The majority of the sample were employed full-time (61.3%), 22.5% were employed part-time, and 16.2% were unemployed. Household income was somewhat positively skewed with 39.6% reporting income of less than $50,000, 35.4% reporting income of $50,000 to $100,000, and 25.0% reported income of greater than $100,000. Most participants reported living in suburban locations (58.3%), followed by urban locations (36.1%), and 5.6% in rural locations.
AYA-F UNCERTAINTY, REPRODUCTIVE DISTRESS, AND AVOIDANCE
The average number of years since treatment was 6.15 (SD = 5.60) ranging from 1 to 23 years. When it came to cancer diagnosis, participants were able to select more than one diagnosis. The most commonly reported diagnosis was leukemia (24.4%), followed by breast cancer (21.6%), Hodgkin lymphoma (18.9%), cervical cancer (7.2%), and non-Hodgkin lymphoma (7.2%). Of the participants who reported their stage of cancer (n =77), the majority of participants reported a stage 2 diagnosis (39.0%). Most participants received more than one treatment. Of the participants who reported their type of cancer treatment (n=107), most received chemotherapy (92.5%), followed by radiation therapy that included the abdominal, pelvic region, or brain (23.4%). Type of treatment was unknown for four participants (3.6%). These medical characteristics are detailed in Table 2. Of the 105 participants that responded to post-treatment reproductive health questions, 93.3% had not been pregnant since cancer treatment, 5.67% were pregnant resulting in a premature delivery, and only one participant was pregnant and had a full-term delivery.
Regarding the main variables of interest, the distributions for scores on the uncertainty scale (URS), reproductive distress scale (RCACS), and the avoidance scale (IES-R) were generally normal for this sample. All scales met the multivariate normality assumptions. The mean of the URS cognitive uncertainty subscale (URS-CU) was 3.05 (SD = 0.63) and emotional uncertainty subscale (URS-EU) was 2.63 (SD = 0.68). The mean of the RCACS score was 60.35 (SD = 10.56). The mean of the IES-R avoidance subscale was 1.61 (SD = 0.88). The mean of the DSE score was 70.46 (SD = 22.90). Focusing on the main outcome variable of interest, item-level analysis for the IES-R (see Table 4) demonstrated that 40.6% of the sample agreed “quite a bit” or “extremely” with the statement, “I am aware that I still have a lot of feelings
AYA-F UNCERTAINTY, REPRODUCTIVE DISTRESS, AND AVOIDANCE
about my fertility, but I don’t deal with them,” which demonstrates that just under half of the sample specifically endorsed avoiding emotions around fertility considerations.
Bivariate Analysis
Correlational analyses were used to examine the association between cognitive and emotional uncertainty (URS), reproductive distress (RCACS), age, age at cancer diagnosis, decisional self-efficacy (DSE), and avoidance (IES-R), as shown in Table 3. A positive correlation was demonstrated between emotional uncertainty and cognitive uncertainty (r = .50, p < .001), and between emotional uncertainty and reproductive distress (r =.44, p < .001). Although age was not demonstrated to significantly correlate with any of the variables of interest except for age at cancer diagnosis (r = .68, p < .001), results show a positive correlation between the outcome variable of avoidance and reproductive distress (r = .32, p < .001), cognitive uncertainty (r = .21, p = 0.024), and emotional uncertainty (r = .27, p = .005). Negative correlations were shown between decisional self-efficacy and avoidance (r = -.33, p < .001), reproductive distress (r = -.30, p = .002), and emotional uncertainty (r = -.23, p = .013).
Main Analyses
Checking Assumptions
Data were examined to check for assumptions necessary for path analyses. Upon examining standardized versions of each of the manifest variables (a variable that can be directly measured), there were no univariate outliers in the dataset and the variables were normally distributed (Bowen & Guo, 2012; Kline, 2015). Covariances were also examined to determine whether the relative scaling of manifest variables would be acceptable to proceed with path
AYA-F UNCERTAINTY, REPRODUCTIVE DISTRESS, AND AVOIDANCE
analyses, during which, some of the covariances showed issues with relative scaling according to Kline’s (2015) cutoff of 10. For this reason, the four variables with the largest variances and scaling (RCACS Total, DSE Mean, age, and age at cancer diagnosis) were transformed by dividing each variable by 10 before including these variables in path analyses. In order to check for multivariate outliers, Mahalanobis Distance values (the distance between a point and a distribution) were generated for all of the manifest variables in the model (Bowen & Guo, 2012). Mahalanobis Distance values were then used to generate associated p values for each case with the cutoff being p < .001 (Bowen & Guo, 2012). No multivariate outliers were identified. Finally, a histogram of standardized residuals generated by conducting a linear regression with all of the manifest variables showed support for multivariate normality (Bowen & Guo, 2012; Kline, 2016). A scatterplot of standardized predicted values and standardized residuals for the model showed no indication of problems with the assumption of homoscedasticity. Tolerance values showed no issues with multicollinearity.
Path Analysis I (Figure 1)
The first path analysis model included only the primary variables of interest (i.e. emotional uncertainty [URS-EU], cognitive uncertainty [URS-CU], reproductive distress [RCACS], and avoidance [IES-R; see Figure 1). The model was just identified (saturated), meaning that no estimates of model fit were generated (Kline, 2015). Results supported the hypothesis that greater emotional uncertainty and greater reproductive distress related to higher levels of avoidance. Specifically, emotional uncertainty predicted reproductive distress (β = 0.47, p < .001) and reproductive distress predicted avoidance (β = 0.26, p = .009). However, there was not a significant direct effect of emotional uncertainty on avoidance (p = .434), indicating a full mediation such that reproductive distress fully explained the association between emotional
AYA-F UNCERTAINTY, REPRODUCTIVE DISTRESS, AND AVOIDANCE
uncertainty and avoidance. Contrary to the hypothesis that reproductive distress would also partially mediate the association between cognitive uncertainty and avoidance, results indicate that cognitive uncertainty was not related to reproductive distress (p = .547) or avoidance (p = .224). In order to examine direct and indirect effects of cases without any missing data (n = 105), bootstrapping (95% bias-corrected confidence intervals and 2000 bootstrap samples) was used. There was not a significant direct effect of emotional uncertainty on avoidance (p = .058). Likewise, there was not a significant direct (p = .390) or indirect (p = .545) effect of cognitive uncertainty on avoidance. However, results continued to show a significant indirect effect of emotional uncertainty on avoidance (β = 0.12, p = .007; 95% CI [0.03, 0.26]). This path model explained 19.7% of the variance in reproductive distress and 13.4% of the variance in avoidance as evidenced by squared multiple correlations (R2).
Post hoc analyses to path analysis I testing the comparative fit index (CFI; > .90) and root mean square error of approximation (RMSEA; < .08) were used to test a more parsimonious model in which non-significant paths were removed so that model fit statistics could be obtained (see Figure 3). The results of the model in which the path between cognitive uncertainty and reproductive distress was removed because it was not significant are consistent with prior findings such that reproductive distress fully mediated the association between emotional uncertainty and avoidance. This parsimonious model achieved excellent fit (χ2 [1] = 0.37, p = .545; CFI = 1.00; RMSEA = 0.00). Within this model, there was a significant effect of emotional uncertainty on reproductive distress (β = 0.44, p < .001) and of reproductive distress on avoidance (β = 0.26, p = .009). All other paths in the model were not significant. In order to examine direct and indirect effects of cases without any missing data (n = 105), the model was run with bootstrapping (95% bias-corrected confidence intervals and 2000 bootstrap samples) for
AYA-F UNCERTAINTY, REPRODUCTIVE DISTRESS, AND AVOIDANCE
the manifest variables in the model. The results from this model indicate that emotional uncertainty has an effect on avoidance that is fully mediated by reproductive distress (i.e., an indirect effect but no direct effect), when controlling for cognitive uncertainty. The model indicates that cognitive uncertainty has no effect on reproductive distress and no effect on avoidance. Squared multiple correlations (R2) showed that the model explained 19.5% of the variance in reproductive distress and 13.7% of the variance in avoidance.
Path Analysis II (Figure 2)
A second path analysis was conducted that included age, age at cancer diagnosis, education, household income, and decisional self-efficacy as control variables selected a priori and based on available research on avoidance. This model was also just identified (saturated), meaning that no estimates of model fit were generated due to not having any degrees of freedom (Kline, 2015). Older age at cancer diagnosis (β = 0.30, p = .008), lower household income (β =-0.21, p = .021), lower self-efficacy (β = -0.22, p = .010), all demonstrated direct effects on higher levels of reproductive distress. Lower self-efficacy was also related to higher avoidance (β = -0.22, p = .020). Emotional uncertainty was demonstrated to be related to reproductive distress (β = 0.39, p < .001), which was slightly attenuated compared to the previous model. No other significant paths were identified in this model.
In order to examine direct and indirect effects for cases without any missing data (n = 90), the model was run with bootstrapping (95% bias-corrected confidence intervals and 2000 bootstrap samples). There was not a significant direct effect of emotional uncertainty on avoidance (p = .766) or of cognitive uncertainty on avoidance (p = .430). There was also not a significant indirect effect of cognitive uncertainty on avoidance (p = .137) or of emotional uncertainty on avoidance (p = .125). The results from this second model with control variables
AYA-F UNCERTAINTY, REPRODUCTIVE DISTRESS, AND AVOIDANCE
indicate that neither emotional uncertainty nor cognitive uncertainty has an effect on avoidance, either directly or mediated through reproductive distress, which did not support the initial hypothesis of predicted associations when considering potential impact of the covariates. The model explained 31.8% of the variance in reproductive stress and 20.5% of the variance in avoidance, indicating an improvement in overall predictive utility compared to the previous model. Of all of the tested models, this model had the best predictive power of both reproductive distress and avoidance compared to all four models investigated.
The post hoc analysis done to path analysis II where the paths between cognitive uncertainty and reproductive distress, and any non significant path between the covariates and reproductive distress or avoidance were removed also resulted in similar findings to the previous identified model that included the control variables (see Figure 4). The parsimonious model achieved excellent fit (χ2 [3] = 0.82, p = .845; CFI = 1.00; RMSEA = 0.00). Age at cancer diagnosis (β = 0.17, p = .048) and household income (β = -0.20, p = .026) had a significant effect on reproductive distress. Self-efficacy was also found to have a significant effect both on reproductive distress (β = -0.19, p = .023) and avoidance (β = -0.25, p = .007). There was a significant effect of Emotional Uncertainty on Reproductive Distress (β = 0.36, p < .001) as in the originally identified model with control variables. No other paths between the primary variables of interest were significant in this model. Squared multiple correlations (R2) showed that the model explained 28.9% of the variance in reproductive distress and 18.6% of the variance in avoidance. In order to examine total and indirect effects, the model was run with bootstrapping (95% bias-corrected confidence intervals and 2000 bootstrap samples) and using only cases without any missing data (n = 90). There was not a significant total effect (p = .402) or indirect effect (p = .089) of emotional uncertainty on avoidance. The results from this model
AYA-F UNCERTAINTY, REPRODUCTIVE DISTRESS, AND AVOIDANCE
indicate that emotional uncertainty does not have an effect on avoidance, either directly or mediated through reproductive distress when controlling for other factors included in the model.
Exploratory analysis
Exploratory analyses were conducted to begin to understand aspects of a patient profile and how they experienced avoidance based on uncertainty, reproductive distress, age at time of diagnosis, household income level, education level, cancer type, fertility preservation practices, and decisional self-efficacy. While the prediction that younger age at diagnosis would be associated with higher avoidance was not supported by the results (β = 0.00, p = 0.967; see Figure 2), it did predict reproductive distress (β = 0.30, p = .008) such that older age at the time of diagnosis related to higher levels of distress. Age at the time of the survey was not found to be related to avoidance as hypothesized (β = 0.06, p = .762). Lower income and lower educational attainment were also hypothesized to relate to higher levels of avoidance, but this hypothesis was not supported for household income (β = -0.09, p = .397) or education (β =- 0.17, p = .095). Related to cancer type and fertility preservation practices, it was hypothesized that those with cervical, ovarian, or uterine/endometrial cancer would express higher levels of avoidance than those with other cancer types, and that those who did not undergo fertility preservation would be more likely to report avoidant tendencies. Cancer type did not relate to avoidance (F[11,99] = 1.05, p = .410) or reproductive distress (F[11,96] = 0.996, p = .456). Interestingly, Non-Hodgkin Lymphoma was significant as a correlate (β = 1.09, t[99] = 2.11, p = .037), but the model did not pass the omnibus F test, so this finding should be interpreted cautiously. There was not a significant difference in avoidance scores between those who underwent fertility preservation and those who did not (t[43] = 0.65, p = .520), and avoidance was not related to cognitive uncertainty (t[63] = 1.964, p = .054) or emotional uncertainty (t[63] = 1.801, p = .077).
AYA-F UNCERTAINTY, REPRODUCTIVE DISTRESS, AND AVOIDANCE
Finally, those with higher levels of perceived decisional self-efficacy were hypothesized to have lower levels of avoidance, which was supported by the results (β = -0.22, p = .020). Overall, age at the time of the survey, age at the time of diagnosis, income level, education level, cancer type, and fertility preservation history were not related to avoidance.
Examining individualized item analysis revealed that several questions from each scale of interest (i.e., URS-EU, RCACS, DSE) were correlated with avoidance. These three specific scales were chosen based on being the variables that were demonstrated to have an association with avoidance in the path analyses. From the emotional uncertainty subscale of the URS (URS-EU), four of the five emotional uncertainty questions were found to be correlated with avoidance (p = .005-.034). The questions that were demonstrated to have a correlation were: “I get worried when a situation is uncertain,” “uncertainty frightens me,” “when uncertain about what to do next, I tend to feel lost,” and “when I can’t clearly discern situations, I get apprehensive.” The only question from the URS emotional uncertainty subscale that did not demonstrate a correlation was “I feel anxious when things are changing.” The reproductive concerns after cancer scale (RCACS) also had several items that showed a significant correlation to avoidance (p = <.001-.037). The seven out of eighteen questions on the RCACS that were significant were: “I am worried about passing on a genetic risk for cancer to my children,” “I worry about telling my (potential) spouse/partner that I may be unable to have children,” “I am scared of not being around to take care of my children someday,” “I am worried about how my family history might affect my children’s health,” I worry that getting pregnant (again) would take too much time and effort,” “the thought of telling my (potential) spouse/partner that I may be unable to have children makes me uncomfortable,” and although considered moderate, the biggest effect size of all demonstrating the most association with avoidance (r = 0.32, p = <.001)
AYA-F UNCERTAINTY, REPRODUCTIVE DISTRESS, AND AVOIDANCE
was “it is stressful to think about trying to get pregnant (again).” From the decisional self-efficacy scale (DSE), seven of the eleven questions were demonstrated to be correlated with avoidance (p = <.001-.010). The three questions that demonstrated moderate, but highest correlation with avoidance (r = -0.33 – -0.31, p = <.001), were: I feel confident that I can “ask questions without feeling dumb,” “ask for advice,” and “figure out the choice that best suits me”
Chapter V
DISCUSSIONS AND CONCLUSION
While existing literature has demonstrated that avoidance is impacted by trait anxiety, interpersonal support systems, risk perception, gender, intersecting social determinants, and self-efficacy in coping (Aldaz et al., 2019; Chae, 2016; Hua & Howell, 2020; Jung et al., 2013; Lipsey & Shepherd et al., 2019; McCloud et al., 2013; Orom et al., 2021; Sweeney et al., 2010), this novel research study sought to better understand the complexities of how emotional uncertainty, cognitive uncertainty, reproductive distress, age, age at diagnosis, household income, education level, and decisional self-efficacy impacted avoidance as a coping technique employed particularly by AYA-F’s. The demonstrated results will be discussed in terms of their clinical utility and the consistency or inconsistency with existing literature, as both were demonstrated. Impact of Emotional Uncertainty
The original path models without control variables (see Figures 1 and 3) did not support the hypothesis that reproductive distress would have a partial mediating effect on the association between emotional uncertainty and avoidance, as a full mediation was observed such that reproductive distress must be present for emotional uncertainty to be linked to avoidance. Also contrary to the hypothesis, neither emotional nor cognitive uncertainty had a direct association with avoidance, and reproductive distress did not mediate the association between cognitive
AYA-F UNCERTAINTY, REPRODUCTIVE DISTRESS, AND AVOIDANCE
uncertainty and avoidance. The key takeaway from these results is that emotional uncertainty had an association with avoidance through reproductive distress, when cognitive uncertainty did not. This indicates that when uncertainty is experienced in the affective realm, it uniquely impacts reproductive distress levels, and thus avoidance levels. This is a critical finding because it offers empirical data into which patients are more likely to avoid in the face of the inherent reproductive distress that comes with family building in survivorship based on how they assess and experience uncertainty. The identification of variables that may lead to avoidant participants is essential for this specific sample (who identified as uncertain or affirmative in the desire to have children in survivorship) because if enacted for an extended time, avoidance can cause an AYA-F to miss their already narrowed window of reproductive viability or to lose their chance to prepare for the challenges of family building after cancer. This initial investigation of the primary psychological variables of interest would suggest that AYA-F’s who report emotional uncertainty would benefit from proactive support services to help them alleviate potential reproductive distress with the goal of ultimately mitigating avoidant behaviors, more so than AYA-F who endorse cognitive uncertainty.
The finding that emotional uncertainty is associated with avoidance through reproductive distress while cognitive uncertainty is not contributes a novel element to the existing literature on uncertainty as it pertains specifically to reproductive distressing information. Research by Greco & Roger (2001) reported that emotional uncertainty can lead to more maladaptive coping while cognitive uncertainty is more likely to result in “tolerance of ambiguity” (p. 530). When applied to those experiencing reproductive distress, AYA-F’s who experience cognitive uncertainty may be more likely to seek out information or able to tolerate the unknowing of fertility impact instead of employing an avoidant coping style like those who endorse emotional uncertainty. As
AYA-F UNCERTAINTY, REPRODUCTIVE DISTRESS, AND AVOIDANCE
we have identified avoidance over time as problematic for this sample due to the implications on the fertility window and decision-making process, this research confirms the literature denoting the relationship between emotional uncertainty and avoidance as maladaptive while adding in the influence of reproductive distress. This is a key finding when investigating avoidant behaviors in AYA-F’s because of the common impact on fertility in this population (Ford et al., 2013; Logan et al., 2019), so understanding avoidant responses to uncertainty in this realm is important clinical and theoretical information to consider.
While uncertainty has been identified as a predominant psychosocial experience for those with chronic illness by the uncertainty management theory, it is posited to be experienced as positive and/or negative depending on an individual’s assessment of the uncertain circumstance (Brashers et al., 2003; Mishel, 1990; Woodgate & Denger, 2002). It could be deduced from the study’s findings that cognitive uncertainty was experienced as “positive” with a tolerance to ambiguity of fertility impact as it was demonstrated to not lead to increased avoidance, which has been conceptualized as maladaptive for this sample. This positive perception of cognitive uncertainty may have led to information seeking or tolerance of ambiguity, instead of avoidance. Perhaps the association seen between emotional uncertainty and avoidance in light of reproductive distress could be explained by participants wanting to avoid further family building considerations or information as a way to either maintain hope (positive outcome of emotional uncertainty) or as a way to avoid something that could be triggering or distressing emotionally (negative outcome of emotional uncertainty), as suggested by previous research (Carcioppolo et al., 2016). Although it is not specified whether the perception of emotional uncertainty was appraised by our sample as positive or negative, the likelihood to avoid when experiencing emotional uncertainty was increased in our sample when compounded by reproductive distress.
AYA-F UNCERTAINTY, REPRODUCTIVE DISTRESS, AND AVOIDANCE
It is important to interpret the results from these path models because they focus on the original variables of interest sought out to be investigated by this study. The results add to literature on uncertainty’s association with avoidance in the face of reproductive distress, which has not been previously investigated to this author’s knowledge. Additionally, reducing emotional uncertainty was found to be important for reducing reproductive distress, which is an important clinical consideration in and of itself. This is imperative information to understand as uncertainty and reproductive distress have been demonstrated to be common experiences in AYA-F survivorship (Benedict et al., 2020; Brashers, 2001; Donovan et al., 2015; Hua and Howell, 2020; Shay et al., 2017; Shay et al., 2018; Wong et al., 2017), and mitigating avoidance in light of these variables is important to allow those who would like to build a family in survivorship to be able to do so in a timely manner.
Impact of Decisional Self-Efficacy
When controlling for age, age at diagnosis, education level, household income, and decisional self-efficacy (see Figures 2 & 4), the mediating association of reproductive distress observed between emotional uncertainty and avoidance disappeared, which does not support the initial hypotheses. Investigation into which control variable had an effect on avoidance demonstrated that decisional self-efficacy emerged as predictive of avoidance, such that decreased decisional self-efficacy was associated with increased reproductive distress and avoidance. These findings mean that those with lower decisional self-efficacy have a lower belief in their ability to make decisions, which increases their reproductive distress as well as the tendency to employ avoidant behaviors.
As defined by Bandura (1994), self-efficacy development is influenced by four major psychological processes: cognitive, motivational, affective and selection processes. This broad
AYA-F UNCERTAINTY, REPRODUCTIVE DISTRESS, AND AVOIDANCE
conceptualization of self-efficacy would position decisional self-efficacy as measured in this study under the selection process, which includes the choices people make based on their self-efficacy beliefs around their ability to handle the decision-making process and associated outcomes (Bandura, 1994). Although decisional self-efficacy was focused on in this study, literature on the larger concept of self-efficacy was drawn upon given the limited literature on decisional self-efficacy specifically. For example, existing literature indicates that people with lower perceived self-efficacy in their coping abilities (affective process) avoid information that may be triggering more often (Hua & Howell, 2020; Orom et al., 2021), consistent with the negative correlation found in the current study when extrapolating decisional self-efficacy results into the broader definition and available research on self-efficacy as a whole. Current literature on self-efficacy and avoidance also points to the impact a person’s assessment of risk level has on the behavioral response (cognitive processes), dependent in part on their self-efficacy of coping abilities (Aldaz et al., 2019; Orom et al., 2021; Shi, 2019).
Although not the intended focus of this study, these path models with covariates tell us clinically that when AYA-F’s feel capable of handling decision making, they demonstrate less reproductive distress and avoidance. This implicates decisional self-efficacy as one of the potential key factors in determining likelihood to use avoidance as a coping strategy. These results are important to interpret because the path models with covariates included were found to have the strongest statistical predictive utility and the results indicate that decisional self-efficacy accounts for increased avoidance over any of the other measured variables. This finding alerts providers to the importance of decisional self-efficacy in this population as a main variable to consider and empower when trying to mitigate the risk of avoidance.
Impact of Additional Covariates
AYA-F UNCERTAINTY, REPRODUCTIVE DISTRESS, AND AVOIDANCE
Results indicated that age at the time of diagnosis and household income were associated with reproductive distress, but not avoidance. While age at the time of diagnosis was positively correlated with reproductive distress indicating that AYA-F’s diagnosed at an older age had increased reproductive distress, household income was negatively correlated with reproductive distress meaning that those with less income reported higher reproductive distress. This negative association of household income with reproductive distress is in line with literature that implicates high financial responsibility related to reproductive methods, surrogacy, or adoption as potential stressors for AYA-F’s (Benedict et al., 2020). Clinically, this is an interesting finding, as these results are further evidence of the income considerations related to fertility and family building that can add to distress levels, which should be addressed both from a larger policy and more individualized support level to lessen the personal financial burden and concern placed on survivors in order to minimize reproductive distress.
Pertaining to age at diagnosis and reproductive distress, the findings were not fully supportive of the research that implicates younger chronological age at the time of diagnosis as leading to more distress and turmoil in survivorship due to unmet fertility information needs (Shay et al., 2017). While reproductive distress is not synonymous with the experience of distress overall, it is interesting to note that the sample studied differs from the available literature in that those who were older at the time of diagnosis had increased reproductive distress. However, these findings make sense in clinical practice because those that are older at the time of diagnosis may already be thinking of fertility and family building considerations as developmentally and biologically appropriate in young adulthood which may cause distress leading to avoidance as a coping mechanism. Also, because AYA-F’s are younger than many of
AYA-F UNCERTAINTY, REPRODUCTIVE DISTRESS, AND AVOIDANCE
the adults diagnosed with cancer, perhaps anyone within the AYA range are categorized as
“younger chronological age.”
Scale Item Analysis Impact
The exploratory item analysis of the URS, RCACS, and DSE demonstrated that there were several specific questions from each scale that were correlated with avoidance (IES-R). The following URS question was most strongly correlated with increased avoidance: “uncertainty frightens me.” It is important to investigate the clinical implications of these associations because it provides insight into affective processes that may lead to avoidance. Additionally, the question from the RCACS scale that showed most significance with relation to avoidance (i.e., “it is stressful to think about trying to get pregnant (again)”) suggests that the mere consideration of pregnancy after treatment may cause reproductive distress ultimately leading to avoidance, which is problematic for this sample who expressed the potential or undecided desire to have children. This positive correlation between URS and RCACS with the IES-R demonstrates an existing relationship between avoidant behaviors and perceptions of a stressful fertility related consideration for AYA-F’s. The DSE results indicated that the following statements were most strongly associated with decreased reports of avoidance: I feel confident that I can “ask questions without feeling dumb”, I feel confident that I can “ask for advice, and I feel confident that I can “figure out the choice that best suits me.” These associations highlight the importance of survivors feeling that they are capable of reaching out for support and making decisions in order to be actively involved in their own care and not avoid healthcare discussions. These findings provide further justification for helping AYA-F’s navigate family building discussions so they do not have to assume the sole responsibility of working through these emotions, distress, and considerations alone.
AYA-F UNCERTAINTY, REPRODUCTIVE DISTRESS, AND AVOIDANCE
As seen in the individual item analysis conducted, some of the survey questions pertaining to significant emotional uncertainty, distress, and avoidance around disclosing fertility risks or fears to partners are also demonstrated in current literature. In the reproductive concerns after cancer scale (RCACS), two of the endorsed questions associated with avoidance were “I worry about telling my (potential) spouse/partner that I may be unable to have children” and “the thought of telling my (potential) spouse/partner that I may be unable to have children makes me uncomfortable.” This alignment of the personal and relational components that could impact an AYA-F is also demonstrated in the research about the tripartite model of uncertainty and regarding identity development within the AYA-F age range (Benedict et al., 2020; Beyers & Seiffge-Krenke, 2010; Logan et al., 2018). Findings suggest that the sample within this study also endorsed similar relational impacts to their levels of avoidance and reproductive distress, which may clinically implicate additional supports and education for the family system as a whole
Implications
This research is critical to help inform practice moving forward as the association between emotional and cognitive uncertainty, reproductive distress, age, age at diagnosis, household income, education level, decisional self-efficacy, and avoidance is now better understood. By having an understanding of this sample’s responses to uncertainty and reproductive distress when controlling for identified risk factors for avoidance, the components that are most significantly associated with avoidance are now more narrowly identified. Through this nuanced understanding, screening practices can be informed, more in-depth knowledge on the AYA-F fertility related survivorship experience is unearthed, and practitioners can utilize this new information to help tailor support services in a way that is individualized to their patients’
AYA-F UNCERTAINTY, REPRODUCTIVE DISTRESS, AND AVOIDANCE
identifiers, while also being versed in understanding associations between types of coping and associated behavioral responses.
While not to strictly profile all patients in the population into the characteristics identified in this study associated with avoidance, the results do allow for increased awareness of which factors might predispose an AYA-F survivor to avoidance. This research clearly demonstrates that those who endorse low decisional self-efficacy are likely to also endorse avoidance. This knowledge can lead to an informed screening process by identifying which factors are and are not associated with avoidant behaviors. For example, given the results, a profile of an AYA-F that is most likely to avoid is beginning to take shape and might present with one or multiple of the following characteristics: high emotional uncertainty and reproductive distress, and/or lower reports of self-efficacy. Knowing these factors associated with avoidance alerts a care team to those that might be at highest risk for avoiding fertility or family building related discussions which is important given that this sample indicated the possible preference to have children in survivorship, which makes avoidance contraindicated to their long-term goals. These results indicate the need to investigate how providers can help facilitate discussions that AYA-F’s may not feel ready for or capable of as a way to help them promote their stated goal of achieving motherhood before avoidance causes them to miss their narrowed window of reproductive viability. Understanding such AYA-F’s tendencies and responses to various factors in survivorship allows providers to be informed, individualized, and proactive in our support efforts.
It is also helpful clinically to know that through reproductive distress, emotional uncertainty is associated with avoidance, but not cognitive uncertainty. This is an important distinction because it can help providers identify between adaptive and potentially maladaptive
AYA-F UNCERTAINTY, REPRODUCTIVE DISTRESS, AND AVOIDANCE
responses to uncertainty as it pertains to reproductive distress. Additionally, it is also important to recognize that household income and age at time of diagnosis are negatively correlated with reproductive distress. This would alert providers to be particularly attuned to the reproductive distress levels of those with low income and who are at an older age. Knowing these identified characteristics allow for deeper understanding of who to proactively support in an effort to minimize stress and/or maladaptive behaviors in survivorship.
Another way to incorporate the results of this study into practice moving forward would be to intentionally build in opportunities to foster opportunities for decisional self-efficacy empowerment into survivorship care to lessen a patient’s emotional uncertainty, reproductive distress, and avoidance. This inflection point could provide assistance with incorporating decisional self-efficacy into an AYA-F’s developing identity. A provider equipped with this knowledge could support survivors by reminding them that they have faced uncertainty before in relation to their initial cancer diagnosis, that they were able to move through that experience that was likely challenging emotionally and mentally, and that they made it into survivorship in an effort to build self-efficacy in general (Bandura, 1994). This approach may help clinicians to empower AYA-F’s with the sense of overall and decisional self-efficacy, that they are capable of managing family building and fertility related experiences, and engaging in relational or medical discussions that may cause emotional uncertainty or reproductive distress.
As demonstrated by the literature and promoted by the American Society for Clinical Oncology and the American Society for Reproductive Medicine, the responsibility of initiating fertility related discussions and support in survivorship should fall on the providers and systems in place treating AYA-F’s (American Cancer Society, 2020; Quinn et al., 2016; Young et al., 2019). We now have additional empirical evidence supporting the need for nuanced support for
AYA-F UNCERTAINTY, REPRODUCTIVE DISTRESS, AND AVOIDANCE
this unique subset of survivors who could benefit from developmentally tailored education and supports initiated by survivorship providers, especially for those survivors who endorse emotional uncertainty, heightened reproductive distress, and/or low decisional self-efficacy.
Limitations
This cross-sectional data analysis presents several limitations. First, the cross-sectional nature of the results only captures the sample’s feelings and impressions of their experience at one point in time, which limits the potential cause and effect of the associated variables. Causal inferences of the data would require a follow up with the same sample over time. The results should be interpreted with the lens that these findings could be representative of just this sample at this point in time, so it cannot be assumed that age and developmental interpretations are not impacted by generational or cohort effects.
The goal of this study was to better understand avoidant coping as it relates to AYA-F’s experience with uncertainty and reproductive distress. Considering the main outcome variable of interest, it is of relevance to note that avoidance was demonstrated to be of average level within the studied sample. The sample, on average, reported moderate levels of avoidance (1.61 [SD = 0.88] out of 3.75). While “normal or typical” avoidance levels are not specified in the existing literature for AYA-F’s, this is important to note when investigating these results because this was not a sample who reported skewed high levels of avoidance as measured by the IES-R subscale which may impact the associations with other variables. Despite the low-average levels of avoidance in this sample, which may still present as clinically problematic, over 33.3% of participants still agreed “quite a bit or extremely” with each of the statements that “I try not to think about my fertility or any problems I might have,” “I am aware that I still have a lot of feelings about my fertility, but I don’t deal with them,” and “I try not to think about my fertility
AYA-F UNCERTAINTY, REPRODUCTIVE DISTRESS, AND AVOIDANCE
or problems I might have in the future.” These item level statistics implicate avoidance as a coping technique employed by at least a third of the sample.
In the context of clinical practice, it is important to acknowledge the homogeneity in the socio-demographics of this sample when interpreting the results and the potential applicability to the larger population. The predominant socio-demographic profile of the sample is as follows: approximately 30 years old at the time of survey, with the average age at diagnosis being 24 years old, having taken the survey approximately 6 years post treatment, White, non-Hispanic/Latinx, college graduates, employed full time, a household income of >$100,000, and living primarily in the suburbs. It is noted that this sample is predominantly White college educated individuals, which may have an impact on their experiences within the healthcare systems in general and regarding their available resources (e.g., both internal and material). As it relates to potential systemic biases, this predominantly White sample may have experienced less uncertainty or distress secondary to working within a system that is not demonstrated to show as much bias towards White identified individuals (Hall et al., 2015). Additionally, the fact that they were predominantly college educated may also influence their overall medical literacy and decisional self-efficacy levels, which could have a direct or indirect impact on their uncertainty type, level of distress, and tendency to avoid.
Regarding additional generalizability considerations, it is important to note that only those assigned female at birth (AFAB) were recruited to partake in this study. Although currently medically and biologically relevant as only AFAB individuals can carry a pregnancy at this time and endure unique treatment related fertility risks, this inclusion criteria is not inclusive of all gender identities and may not be representative of the experience for all those who self-identify as AYA-F. Additionally, it could be argued that it is a particularly Westernized view to interpret
AYA-F UNCERTAINTY, REPRODUCTIVE DISTRESS, AND AVOIDANCE
information seeking (opposite of avoidance) and individualized decisional self-efficacy around family building as being a “positive” coping mechanism. Perhaps a more collectivistic approach to family building discussions is culturally appropriate for an individual meaning that lower levels of decisional self-efficacy or personal avoidance may not be maladaptive for someone more likely to defer to the larger family system. Finally, although participants from this sample were recruited nationally, international participants were excluded so the results may not be applicable to a global population.
An additional limitation to this study is related to the measures that were included in the original questionnaire as it was not designed with the specific intention to investigate associations between uncertainty, reproductive distress, and avoidance. Specifically, both the uncertainty response scale (URS) and the impact of events scale revised (IES-R) were not specifically normed for fertility related stressors in healthcare or with the AYA-F population (Greco & Roger, 2001; Horowitz et al., 1979; Weiss, 2007). The IES-R was originally created to assess PTSD symptoms and is described generally as a measure to assess the subjective impact of a distressing event (Weiss, 2007). To account for this gap in the intended avoidance focus related to the IES-R, the creators of the survey utilized in the original study of this sample indicated in the instructions for the IES-R to “please think about your fertility and possible fertility problems you might have in the future” when answering the questions, which may lessen this possible limitation. However, with the URS, the survey asks participants how they respond to “uncertainty in their life,” not necessarily related to fertility and family building, thus the measure assessed trait-like tendencies for managing uncertainty. Additionally, the URS does not specifically pertain to uncertainty around illness although the instructions on the survey preface the questions by saying “people sometimes have difficulty facing uncertain situations, such as
AYA-F UNCERTAINTY, REPRODUCTIVE DISTRESS, AND AVOIDANCE
worrying about their health or their future.” This discrepancy in the intended population and focus of the original measures not being related to healthcare may impact the power of the observed associations and correlations seen with both emotional and cognitive uncertainty. In relation to self-efficacy, the DSE specifically assesses decisional self-efficacy. Although there is evidence in the literature that this falls under self-efficacy in general, it could have been more beneficial to use a measure specifically assessing general self-efficacy related to reproductive distress to better understand the experiences of this nuanced population. Additionally, as this study did not set out to specifically do measure construction or analysis, it is untraditional to do correlational item analysis for each of the variable scales (URS, RCACS, and DSE) with avoidance. While this analysis did provide insight into AYA-F’s thought processes and is further research/hypothesis generating, the practice of correlating individual questions with the construct of avoidance must be identified as a limitation.
Finally, as this was a secondary study of archival data, not all known control variables for avoidance were collected. For example, relational support levels, familial communication patterns, partnership status, and trait anxiety are known factors that impact likelihood to avoid (Aldaz et al., 2019; Chae, 2016; Hua & Howell, 2020; Jung et al., 2013; Lipsey & Shepherd et al., 2019; McCloud et al., 2013; Orom et al., 2021; Sweeney et al., 2010), but were not assessed in the existing questionnaire. Also, the literature predominantly addressed self-efficacy in coping, while the decisional self-efficacy (DSE) scale was particularly centered around one’s confidence in their ability to make decisions either independently or with a provider which has an impact on overall self-efficacy. While decisional self-efficacy could be interpreted as related to self-efficacy in coping and self-efficacy more broadly, there may be a slight distinction between the definitions that could also impact the interpretation of the results.
AYA-F UNCERTAINTY, REPRODUCTIVE DISTRESS, AND AVOIDANCE
Suggestions for Future Research
Given the findings, identified gaps, and limitations in the current research, there are several areas of interest for future research. One such avenue for future research would be to dive deeper into decisional self-efficacy and how it interplays with emotional uncertainty as it relates to avoidance as well as how it empirically relates to both decisional self-efficacy and self-efficacy in its most broad definition around specifically managing reproductive distress (i.e., PROMIS scale). This study found that decisional self-efficacy was significantly associated with emotional uncertainty, reproductive distress, and avoidance, which was the most robust of any of the covariates that were investigated. The results of this study may help with hypothesis generating in future research such that both emotional uncertainty and self-efficacy matter when assessing avoidant behaviors, but the relationship needs to be investigated further. Future research may also explore whether opportunities within survivorship to increase decisional self-efficacy may have an influence on building an AYA-F’s identity and confidence in managing reproductive distress and emotional uncertainty instead of turning to avoidance as a coping mechanism. Although research clearly links self-efficacy and resilience with the ability to face distress (Chiesi et al., 2022), additional research is required on how to maximize ways to build self-efficacy in AYA-F’s considering family building.
With the results from this study, more information is now known regarding the initial formulation of a profile of AYA-F who is likely to endorse avoidance. These data are important when trying to maximize the family building discussion opportunities prior to fertility windows further closing before family building options are explored. Additional analysis is necessary to better parse out this profile, but the results begin to inform the initial profile of such patient. The item analysis done on the URS, RCACS, and DSE also generates further research
AYA-F UNCERTAINTY, REPRODUCTIVE DISTRESS, AND AVOIDANCE
possibilities regarding identifying specific screening questions that would be most predictive of such avoidant behaviors. It could also be interesting to research what kind of support services are most helpful for this population or “profile” of patient, what supports would empower decisional self-efficacy and self-efficacy broadly, and at what time in treatment or survivorship these services should be delivered in order to optimize the impact. Additionally, if an AYA-F is avoiding as a way of managing their distress or uncertainty, research into how support services could overcome avoidance of services would also be essential. Given the results of this research, it is important to keep the developmental stages and identities of AYA-F’s in consideration as well when creating tailored services. Future research investigating how to best address the needs of AYA-F’s at different ages at time of diagnosis, age at time of family building consideration, and the developmental readiness for addressing fertility and family building is also essential to better inform practice.
Finally, it would be helpful to dive deeper into avoidance in the AYA-F population to better understand the behaviors of those who avoid as a way to empirically identify the threshold that transitions avoidance from useful to manage distress, to a maladaptive level. Again, avoidance is known to be an effective and useful coping strategy in the short term for managing distress, however, risk associated with avoidance for AYA-F’s wanting to build a family in survivorship comes into play when employed in the long term due to potentially missing an already narrowed reproductive window which would further limit an AYA-F’s ability to have a biologically-related child if desired or when avoidance leads to being unprepared for potential family building challenges via reproductive medicine or adoption. To this author’s knowledge, there is a dearth of longitudinal studies that investigate the impacts of avoidance specifically within the AYA-F survivorship population. Investigation into the sequelae of healthcare and
AYA-F UNCERTAINTY, REPRODUCTIVE DISTRESS, AND AVOIDANCE
mental health impacts of avoidance could further bolster the argument for needing to proactively identify and support AYA-F’s with a tendency to avoid.
Conclusion
In conclusion, this novel research confirmed that AYA-F survivors experience uncertainty, reproductive distress, and avoidance in survivorship due to a myriad of factors. While avoidance can be adaptive in the short term as a coping mechanism to manage reproductive distress or uncertainty, there are medical contraindications to avoidance of fertility and family building considerations for AYA-F survivors potentially desiring to have a family during survivorship. It was concluded that reproductive distress impacts how AYA-F’s experience emotional uncertainty and avoidance, that age at the time of diagnosis and household income impact reproductive distress levels, and that decisional self-efficacy impacts both reproductive distress and avoidance.
All of these findings help compile a preliminary profile of AYA-F’s with low decisional self-efficacy as most likely to employ avoidance in survivorship in the face of emotional uncertainty and reproductive distress, which ultimately informs providers of who to offer targeted support services to in order to optimize family building opportunities for those interested during survivorship. More targeted research is necessary in order to better understand how and when support would be most effective for AYA-F’s. This study also assisted in adding to existing literature on the variables of interest and generated several new hypotheses for future research to better understand the nuances experienced by AYA-F’s looking to build families after a cancer diagnosis.
AYA-F UNCERTAINTY, REPRODUCTIVE DISTRESS, AND AVOIDANCE
Chapter VI
REFERENCES
Aldaz, B. E., Hegarty, R. S. M., Conner, T. S., Perez, D., & Treharne, G. J. (2019). Is avoidance of illness uncertainty associated with distress during oncology treatment? A daily diary
study. Psychology & Health, 34(4), 422–437.
https://doi.org/10.1080/08870446.2018.1532511
American Cancer Society (2020). Cancer Facts and Figures. Special Section: Cancer in Adolescents and Young Adults.
https://www.cancer.org/content/dam/cancer-org/research/cancer-facts-and-statistics/annua
l-cancer-facts-and-figures/2020/special-section-cancer-in-adolescents-and-young-adults-2
020.pdf
Arbuckle, J. L. (2021). Amos (Version 28.0) [Computer Program]. IBM SPSS.
Arbuckle, J. L. (2021a). Amos 28 user’s guide. IBM SPSS.
Bandura, A. (1994). Self-efficacy. In V. S. Ramachaudran (Ed.), Encyclopedia of human behavior (Vol. 4, pp. 71-81). New York: Academic Press.
Barbour, J. B., Rintamaki, L. S., Ramsey, J. A., & Brashers, D. E. (2012). Avoiding Health Information. Journal of Health Communication, 17(2), 212–229.
https://doi.org/10.1080/10810730.2011.585691
Baron, R. M., & Kenny, D. A. (1986). The moderator-mediator variable distinction in social psychological research: Conceptual, strategic, and statistical considerations. Journal of
Personality and Social Psychology, 51, 1173-1182.
AYA-F UNCERTAINTY, REPRODUCTIVE DISTRESS, AND AVOIDANCE
Barton, S. E., Najita, J. S., Ginsburg, E. S., Leisenring, W. M., Stovall, M., Weathers, R. E., Sklar, C. A., Robison, L. L., & Diller, L. (2013). Infertility, infertility treatment, and achievement of pregnancy in female survivors of childhood cancer: A report from the Childhood Cancer Survivor Study cohort. The Lancet Oncology, 14(9), 873–881.
https://doi.org/10.1016/S1470-2045(13)70251-1
Becker, T. E., Atinc, G., Breaugh, J. A., Carlson, K. D., Edwards, J. R., & Spector, P. E. (2016). Statistical control in correlational studies: 10 essential recommendations for
organizational researchers. Journal of Organizational Behavior, 37(2), 157-167.
Becker, T. E. (2005). Potential problems in the statistical control of variables in organizational research: A qualitative analysis with recommendations. Organizational Research Methods, 8(3), 274-289.
Benedict, C., Hahn, A. L., McCready, A., Kelvin, J. F., Diefenbach, M., & Ford, J. S. (2020). Toward a theoretical understanding of young female cancer survivors’ decision-making about family-building post-treatment. Supportive Care in Cancer, 28(10), 4857–4867. https://doi.org/10.1007/s00520-020-05307-1
Benedict, C., Hahn, A. L., Diefenbach, M. A., & Ford, J. S. (2019). Recruitment via social media: advantages and potential biases. Digital Health, 5, 1-11. Benedict, C., Shuk, E., & Ford, J. S. (2016). Fertility Issues in Adolescent and Young Adult Cancer Survivors. Journal of Adolescent and Young Adult Oncology, 5(1), 48–57.
https://doi.org/10.1089/jayao.2015.0024
Beyers, W., & Seiffge-Krenke, I. (2010). Does identity precede intimacy? Testing Erikson’s theory on romantic development in emerging adults of the 21st century. Journal of Adolescent Research, 25(3), 387-415.
AYA-F UNCERTAINTY, REPRODUCTIVE DISTRESS, AND AVOIDANCE
Bowen, N., & Guo, S. (2012). Structural equation modeling: Pocket guides to social research methods. Oxford University Press.
Brashers, D. E. (2001). Communication and Uncertainty Management. Journal of Communication, 21.
Brashers, D. E., Neidig, J. L., Russell, J. A., Cardillo, L. W., Haas, S. M., Dobbs, L. K., Garland, M., McCartney, B., & Nemeth, S. (2003). The Medical, Personal, and Social Causes of Uncertainty in HIV Illness. Issues in Mental Health Nursing, 24(5), 497–522. https://doi.org/10.1080/01612840305292
Byrne, B. (2016). Structural Equation Modeling with AMOS (3rd ed.). New York, NY: Routledge.
Bunn, H. & O’Connor, A.M. (1996). Validation of client decision-making instruments in the context of psychiatry. Canadian Journal of Nursing Research, 28(3), 13–27
Campbell, A. G., & Hillemeier, M. (2021). Fertility counseling information adequacy as a moderator of regret among adolescent and young adult breast cancer survivors. Supportive Care in Cancer, 29(5), 2689–2697. https://doi.org/10.1007/s00520-020-05771-9
Canzona, M. R., Victorson, D. E., Murphy, K., Clayman, M. L., Patel, B., Puccinelli‐Ortega, N., McLean, T. W., Harry, O., Little‐Greene, D., & Salsman, J. M. (2021). A conceptual model of fertility concerns among adolescents and young adults with cancer. Psycho-Oncology, 30(8), 1383–1392. https://doi.org/10.1002/pon.5695
Carcioppolo, N., Yang, F., & Yang, Q. (2016). Reducing, Maintaining, or Escalating Uncertainty? The Development and Validation of Four Uncertainty Preference Scales Related to Cancer Information Seeking and Avoidance. Journal of Health Communication, 21(9), 979–988. https://doi.org/10.1080/10810730.2016.1184357
AYA-F UNCERTAINTY, REPRODUCTIVE DISTRESS, AND AVOIDANCE
Chae, J. (2016). Who Avoids Cancer Information? Examining a Psychological Process Leading to Cancer Information Avoidance. Journal of Health Communication, 21(7), 837–844. https://doi.org/10.1080/10810730.2016.1177144
Chae, J. (2017). The role of intolerance of uncertainty in the repeated exposure to cancer information. Journal of Psychosocial Oncology, 35(3), 335–345. https://doi.org/10.1080/07347332.2016.1277822
Chae, J., Lee, C., & Jensen, J. D. (2016). Correlates of Cancer Information Overload: Focusing on Individual Ability and Motivation. Health Communication, 31(5), 626–634. https://doi.org/10.1080/10410236.2014.986026
Chiesi, F., Vizza, D., Valente, M., Bruno, R., Lau, C., Campagna, M. R., Lo Iacono, M., & Bruno, F. (2022). Positive personal resources and psychological distress during the COVID-19 pandemic: Resilience, optimism, hope, courage, trait mindfulness, and self-efficacy in breast cancer patients and survivors. Supportive Care in Cancer.
https://doi.org/10.1007/s00520-022-07123-1
Crook, B., Glowacki, E. M., Love, B., Jones, B. L., Macpherson, C. F., & Johnson, R. H. (2016). Hanging by a thread: Exploring the features of nonresponse in an online young adult cancer survivorship support community. Journal of Cancer Survivorship, 10(1), 185–193. https://doi.org/10.1007/s11764-015-0465-8
Donovan, E. E., Brown, L. E., LeFebvre, L., Tardif, S., & Love, B. (2015). “The Uncertainty Is What Is Driving Me Crazy”: The Tripartite Model of Uncertainty in the Adolescent and Young Adult Cancer Context. Health Communication, 30(7), 702–713. https://doi.org/10.1080/10410236.2014.898193
AYA-F UNCERTAINTY, REPRODUCTIVE DISTRESS, AND AVOIDANCE
Ford, J. S., Chou, J. F., & Sklar, C. A. (2013). Attendance at a survivorship clinic: Impact on knowledge and psychosocial adjustment. Journal of Cancer Survivorship, 7(4), 535–543. https://doi.org/10.1007/s11764-013-0291-9
Gorman, J. R., Su, H. I., Pierce, J. P., Roberts, S. C., Dominick, S. A., & Malcarne, V. L. (2014). A multidimensional scale to measure the reproductive concerns of young adult female cancer survivors. Journal of Cancer Survivorship, 8(2), 218–228. https://doi.org/10.1007/s11764-013-0333-3
Gorman, J. R., Standridge, D., Lyons, K. S., Elliot, D. L., Winters-Stone, K., Julian, A. K., Weprin, J., Storksdieck, M., & Hayes-Lattin, B. (2018). Patient-centered communication between adolescent and young adult cancer survivors and their healthcare providers: Identifying research gaps with a scoping review. Patient Education and Counseling, 101(2), 185–194. https://doi.org/10.1016/j.pec.2017.08.020
Gorman, J. R., Pan‐Weisz, T. M., Drizin, J. H., Su, H. I., & Malcarne, V. L. (2019). Revisiting the Reproductive Concerns After Cancer (RCAC) scale. Psycho-Oncology, 28(7), 1544–1550. https://doi.org/10.1002/pon.5130
Greco, V., & Roger, D. (2001). Coping with uncertainty: The construction and validation of a new measure. Personality and Individual Differences, 31(4), 519–534. https://doi.org/10.1016/S0191-8869(00)00156-2
Greco, V., & Roger, D. (2003). Uncertainty, stress, and health. Personality and Individual Differences, 34(6), 1057–1068. https://doi.org/10.1016/S0191-8869(02)00091-0
Hall, W. J., Chapman, M. V., Lee, K. M., Merino, Y. M., Thomas, T. W., Payne, B. K., Eng, E.,
Day, S. H., & Coyne-Beasley, T. (2015). Implicit Racial/Ethnic Bias Among Health Care Professionals and Its Influence on Health Care Outcomes: A Systematic Review.
AYA-F UNCERTAINTY, REPRODUCTIVE DISTRESS, AND AVOIDANCE
American journal of public health, 105(12), 60–76.
https://doi.org/10.2105/AJPH.2015.302903
Halliday, L. E., & Boughton, M. A. (2011). Exploring the concept of uncertain fertility, reproduction and motherhood after cancer in young adult women: Uncertain fertility and motherhood after cancer. Nursing Inquiry, 18(2), 135–142.https://doi.org/10.1111/j.1440-1800.2011.00532.x
Hawkey, A., Ussher, J. M., Perz, J., & Parton, C. (2021). Talking but not always understanding: Couple communication about infertility concerns after cancer. BMC Public Health, 21(1), 161. https://doi.org/10.1186/s12889-021-10188-y
Hayes, A. (2022). Introduction to mediation, moderation, and conditional process analysis: A regression-based approach (3rd Ed.). Guilford Publications.
Hillen, M. A., Gutheil, C. M., Strout, T. D., Smets, E. M. A., & Han, P. K. J. (2017). Tolerance of uncertainty: Conceptual analysis, integrative model, and implications for healthcare. Social Science & Medicine, 180, 62–75. https://doi.org/10.1016/j.socscimed.2017.03.024
Howell, J. L., Ratliff, K. A., & Shepperd, J. A. (2016). Automatic attitudes and health information avoidance. Health Psychology, 35(8), 816–823. https://doi.org/10.1037/hea0000330
Hua, J., & Howell, J. L. (2020). Coping self-efficacy influences health information avoidance. Journal of Health Psychology, 135910532096566. https://doi.org/10.1177/1359105320965664
Iannarino, N. T., & Palmer-Wackerly, A. L. (2021). Fertility Preservation Decision-Making Communication between Young Adult Cancer Patients and Their Romantic Partners: An
AYA-F UNCERTAINTY, REPRODUCTIVE DISTRESS, AND AVOIDANCE
Application of the DECIDE Typology. Health Communication, 1–12.
https://doi.org/10.1080/10410236.2020.1868065
Jung, M., Ramanadhan, S., & Viswanath, K. (2013). Effect of information seeking and avoidance behavior on self-rated health status among cancer survivors. Patient Education and Counseling, 92(1), 100–106. https://doi.org/10.1016/j.pec.2013.02.008
Kline, R. B. (2015). Principles and practice of structural equation modeling. Guilford publications.
Lipsey, N. P., & Shepperd, J. A. (2019). The role of powerful audiences in health information avoidance. Social Science & Medicine, 220, 430–439. https://doi.org/10.1016/j.socscimed.2018.11.037
Logan, S., Perz, J., Ussher, J. M., Peate, M., & Anazodo, A. (2018). A systematic review of patient oncofertility support needs in reproductive cancer patients aged 14 to 45 years of age. Psycho-Oncology, 27(2), 401–409. https://doi.org/10.1002/pon.4502
Logan, S., Perz, J., Ussher, J. M., Peate, M., & Anazodo, A. (2019). Systematic review of fertility-related psychological distress in cancer patients: Informing on an improved model of care. Psycho-Oncology, 28(1), 22–30. https://doi.org/10.1002/pon.4927
Mertens, A. C., & Gilleland Marchak, J. (2015). Mental health status of adolescent cancer survivors. Clinical Oncology in Adolescents and Young Adults, 87. https://doi.org/10.2147/COAYA.S49174
McCloud, R. F., Jung, M., Gray, S. W., & Viswanath, K. (2013). Class, race and ethnicity and information avoidance among cancer survivors. British Journal of Cancer, 108(10), 1949–1956. https://doi.org/10.1038/bjc.2013.182
AYA-F UNCERTAINTY, REPRODUCTIVE DISTRESS, AND AVOIDANCE
McQueen, A., Vernon, S.W., & Swank, P.R. (2013). Construct definition and scale development for defensive information processing: an application to colorectal cancer screening. Health Psychology, 32, 190-202.
Miano, S. J., Douglas, S. L., Hickman, R. L., DiMarco, M., Piccone, C., & Daly, B. J. (2020). Exploration of Decisional Control Preferences in Adolescents and Young Adults with Cancer and Other Complex Medical Conditions. Journal of adolescent and young adult oncology, 9(4), 464–471.
Miller, L. E. (2014). Uncertainty Management and Information Seeking in Cancer Survivorship. Health Communication, 29(3), 233–243. https://doi.org/10.1080/10410236.2012.739949
Mishel, M.H. (1990). Reconceptualization of the uncertainty in illness theory. Journal of Nursing Scholarship, 22, 256–262. https://doi.org/10.1111/j.1547-5069.1990 .tb00225.x
National Cancer Institute. (August 7, 2020). Study Offers Insights on Health Problems among AYA Cancer Survivors. https://www.cancer.gov/news-events/cancer-currents-blog/2020/aya-cancer-survivors-hea lth-problems
National Cancer Institute. (2009). Definition of cancer terms.
http://www.cancer.gov/dictionary?cdrid=450125.
O’Connor, A., M. (2002). User-Manual – Decisional Self-Efficacy Scale. Ottawa. Ottawa Hospital Research Institute.
https://decisionaid.ohri.ca/docs/develop/User_Manuals/UM_Decision_SelfEfficacy.pdf
AYA-F UNCERTAINTY, REPRODUCTIVE DISTRESS, AND AVOIDANCE
Orom, H., Schofield, E., Kiviniemi, M. T., Waters, E. A., & Hay, J. L. (2021). Agency beliefs are associated with lower health information avoidance. Health Education Journal, 80(3), 272–286. https://doi.org/10.1177/0017896920967046
Pillet, S. (2010). Cancer Is One More Milestone. Oncology Nursing Society Connect. March, 8-11.
Quinn, G. P., Woodruff, T. K., Knapp, C. A., Bowman, M. L., Reinecke, J., & Vadaparampil, S. T. (2016). Expanding the Oncofertility Workforce: Training Allied Health Professionals to Improve Health Outcomes for Adolescents and Young Adults. Journal of Adolescent and Young Adult Oncology, 5(3), 292–296. https://doi.org/10.1089/jayao.2016.0003
Sansom-Daly, U. M., & Wakefield, C. E. (2013). Distress and adjustment among adolescents and young adults with cancer: an empirical and conceptual review. Translational Pediatrics, 2(4), 167–197.
Shay, L. A., Parsons, H. M., & Vernon, S. W. (2017). Survivorship Care Planning and Unmet Information and Service Needs Among Adolescent and Young Adult Cancer Survivors. Journal of Adolescent and Young Adult Oncology, 6(2), 327–332. https://doi.org/10.1089/jayao.2016.0053
Shay, L. A., Schmidt, S., Cornell, S. D., & Parsons, H. M. (2018). “Making My Own Decisions Sometimes”: A Pilot Study of Young Adult Cancer Survivors’ Perspectives on Medical Decision-Making. Journal of Cancer Education, 33(6), 1341–1346. https://doi.org/10.1007/s13187-017-1256-x
Shi, W. (2019). Health Information Seeking versus Avoiding: How Do College Students Respond to Stress-related Information? American Journal of Health Behavior, 43(2), 437–448. https://doi.org/10.5993/AJHB.43.2.18
AYA-F UNCERTAINTY, REPRODUCTIVE DISTRESS, AND AVOIDANCE
Shnorhavorian, M., Harlan, L. C., Smith, A. W., Keegan, T. H. M., Lynch, C. F., Prasad, P. K., Cress, R. D., Wu, X.-C., Hamilton, A. S., Parsons, H. M., Keel, G., Charlesworth, S. E., Schwartz, S. M., & AYA HOPE Study Collaborative Group. (2015). Fertility preservation knowledge, counseling, and actions among adolescent and young adult patients with cancer: A population-based study: Fertility Issues and AYA Patients With Cancer. Cancer, 121(19), 3499–3506. https://doi.org/10.1002/cncr.29328
Smits-Seemann, R. R., Kaul, S., Zamora, E. R., Wu, Y. P., & Kirchhoff, A. C. (2017). Barriers to follow-up care among survivors of adolescent and young adult cancer. Journal of Cancer Survivorship, 11(1), 126–132. https://doi.org/10.1007/s11764-016-0570-3
Sweeny, K., Melnyk, D., Miller, W., & Shepperd, J. A. (2010). Information Avoidance: Who, What, When, and Why. Review of General Psychology, 14(4), 340–353. https://doi.org/10.1037/a0021288
Ussher, J. M., & Perz, J. (2019). Infertility-related distress following cancer for women and men: A mixed method study. Psycho-Oncology, 28(3), 607–614. https://doi.org/10.1002/pon.4990
van Dijk, M., van den Berg, M. H., Overbeek, A., Lambalk, C. B., van den Heuvel-Eibrink, M. M., Tissing, W. J., Kremer, L. C., van der Pal, H. J., Loonen, J. J., Versluys, B., Bresters, D., Kaspers, G. J. L., van Leeuwen, F. E., van Dulmen-den Broeder, E., & DCOG LATER-VEVO study group. (2018). Reproductive intentions and use of reproductive health care among female survivors of childhood cancer. Human Reproduction, 33(6), 1167–1174. https://doi.org/10.1093/humrep/dey058
AYA-F UNCERTAINTY, REPRODUCTIVE DISTRESS, AND AVOIDANCE
Weis, D. S. (2007). The impact of event scale: revised. In Wilson, J. P. & So-kum Tang, C. (Eds.), Cross-cultural assessment of psychological trauma and PTSD (pp. 219–238). Springer.
Wenzel, L., Dogan-Ates, A., Habbal, R., Berkowitz, R., Goldstein, D. P., Bernstein, M., Coffey Kluhsman, B., Osann, K., Newlands, E., Seckl, M. J., Hancock, B., & Cella, D. (2005). Defining and Measuring Reproductive Concerns of Female Cancer Survivors. Journal of the National Cancer Institute Monographs, 2005(34), 94–98. https://doi.org/10.1093/jncimonographs/lgi017
Wong, A. W. K., Chang, T., Christopher, K., Lau, S. C. L., Beaupin, L. K., Love, B., Lipsey, K. L., & Feuerstein, M. (2017). Patterns of unmet needs in adolescent and young adult (AYA) cancer survivors: In their own words. Journal of Cancer Survivorship, 11(6), 751–764. https://doi.org/10.1007/s11764-017-0613-4
Woodgate, R. L., & Degner, L. F. (2002). “Nothing is carved in stone!”: Uncertainty in children with cancer and their families. European Journal of Oncology Nursing, 6(4), 191–202. https://doi.org/10.1054/ejon.2002.0220
Woodruff, T. K., Ataman-Millhouse, L., Acharya, K. S., Almeida-Santos, T., Anazodo, A., Anderson, R. A., Appiah, L., Bader, J., Becktell, K., Brannigan, R. E., Breech, L., Bourlon, M. T., Bumbuliene, Ž., Burns, K., Campo-Engelstein, L., Campos, J. R., Centola, G. M., Chehin, M. B., Chen, D., … Zelinski, M. (2021). A View from the past into our collective future: The oncofertility consortium vision statement. Journal of Assisted Reproduction and Genetics, 38(1), 3–15. https://doi.org/10.1007/s10815-020-01983-4
AYA-F UNCERTAINTY, REPRODUCTIVE DISTRESS, AND AVOIDANCE
Young, K., Shliakhtsitsava, K., Natarajan, L., Myers, E., Dietz, A. C., Gorman, J. R., Martínez, M. E., Whitcomb, B. W., & Su, H. I. (2019). Fertility counseling before cancer treatment and subsequent reproductive concerns among female adolescent and young adult cancer survivors. Cancer, 125(6), 980–989. https://doi.org/10.1002/cncr.31862
AYA-F UNCERTAINTY, REPRODUCTIVE DISTRESS, AND AVOIDANCE
Chapter VII
TABLES AND FIGURES
AYA-F UNCERTAINTY, REPRODUCTIVE DISTRESS, AND AVOIDANCE
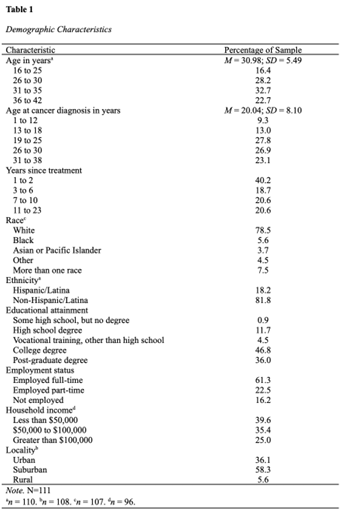
AYA-F UNCERTAINTY, REPRODUCTIVE DISTRESS, AND AVOIDANCE

AYA-F UNCERTAINTY, REPRODUCTIVE DISTRESS, AND AVOIDANCE
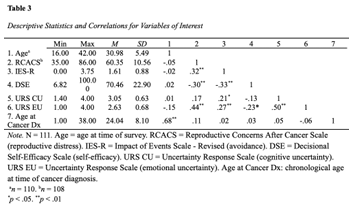
AYA-F UNCERTAINTY, REPRODUCTIVE DISTRESS, AND AVOIDANCE
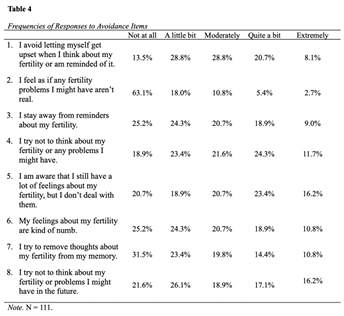
AYA-F UNCERTAINTY, REPRODUCTIVE DISTRESS, AND AVOIDANCE

AYA-F UNCERTAINTY, REPRODUCTIVE DISTRESS, AND AVOIDANCE
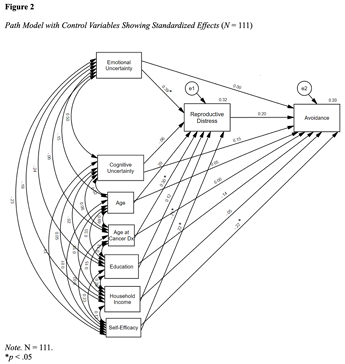
AYA-F UNCERTAINTY, REPRODUCTIVE DISTRESS, AND AVOIDANCE
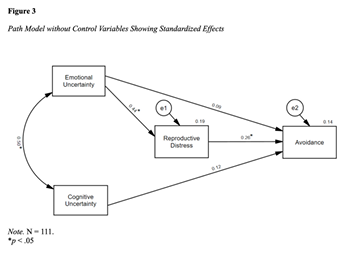
AYA-F UNCERTAINTY, REPRODUCTIVE DISTRESS, AND AVOIDANCE
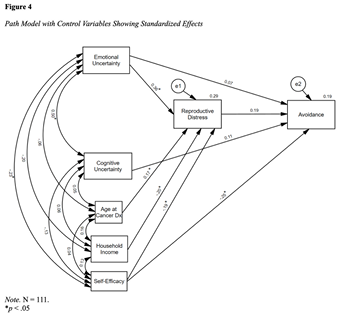
AYA-F UNCERTAINTY, REPRODUCTIVE DISTRESS, AND AVOIDANCE
Chapter 8
APPENDICES
AYA-F UNCERTAINTY, REPRODUCTIVE DISTRESS, AND AVOIDANCE
Appendix A
Socio-Demographic Information
AYA-F UNCERTAINTY, REPRODUCTIVE DISTRESS, AND AVOIDANCE

AYA-F UNCERTAINTY, REPRODUCTIVE DISTRESS, AND AVOIDANCE

AYA-F UNCERTAINTY, REPRODUCTIVE DISTRESS, AND AVOIDANCE
Appendix B
Medical History
AYA-F UNCERTAINTY, REPRODUCTIVE DISTRESS, AND AVOIDANCE
AYA-F UNCERTAINTY, REPRODUCTIVE DISTRESS, AND AVOIDANCE

AYA-F UNCERTAINTY, REPRODUCTIVE DISTRESS, AND AVOIDANCE
Appendix C
Reproductive History
AYA-F UNCERTAINTY, REPRODUCTIVE DISTRESS, AND AVOIDANCE

AYA-F UNCERTAINTY, REPRODUCTIVE DISTRESS, AND AVOIDANCE

AYA-F UNCERTAINTY, REPRODUCTIVE DISTRESS, AND AVOIDANCE
Appendix D
Reproductive Concerns After Cancer Scale (RCACS) (Gorman et al., 2014) Measures reproductive distress variable

AYA-F UNCERTAINTY, REPRODUCTIVE DISTRESS, AND AVOIDANCE

AYA-F UNCERTAINTY, REPRODUCTIVE DISTRESS, AND AVOIDANCE

AYA-F UNCERTAINTY, REPRODUCTIVE DISTRESS, AND AVOIDANCE
Appendix E
Impact of Events Scale – Revised (IES-R) (Weiss, 2007)
Measures avoidance variable
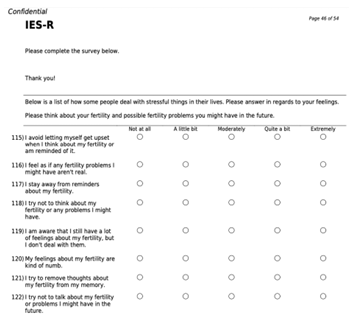
AYA-F UNCERTAINTY, REPRODUCTIVE DISTRESS, AND AVOIDANCE
Appendix F
Decisional Self-Efficacy Scale (DSE) (O’Connor, 2002)
Measures self-efficacy variable
AYA-F UNCERTAINTY, REPRODUCTIVE DISTRESS, AND AVOIDANCE

AYA-F UNCERTAINTY, REPRODUCTIVE DISTRESS, AND AVOIDANCE

AYA-F UNCERTAINTY, REPRODUCTIVE DISTRESS, AND AVOIDANCE
Appendix G
Uncertainty Response Scale (URS) (Greco & Roger, 2001)
(150-154) Measures emotional uncertainty variable
(155-159) Measures cognitive uncertainty variable